Allergy-IBS Risk Assessment Tool
About This Tool
This assessment helps estimate your risk of developing IBS if you have allergic disorders. Based on current research, people with allergic conditions are 2.5 times more likely to develop IBS.
Your Risk Assessment
Key Symptoms to Watch For
Abdominal Pain
Often linked to food allergens or histamine release
Bloating
May be triggered by airborne allergens or dietary factors
Diarrhea
Can result from mast cell activation or histamine overload
Constipation
Often associated with chronic inflammation and gut motility issues
Ever felt a sudden flare‑up after a meal and wondered if it’s just a bad stomach day or something deeper? There’s a growing body of research showing that allergic disorders and Irritable Bowel Syndrome (IBS) often walk hand‑in‑hand. This article unpacks what each condition is, why they overlap, and what practical steps you can take if you’re dealing with both.
What Exactly Are Allergic Disorders?
Allergic disorders are immune‑mediated reactions that occur when the body mistakenly identifies harmless substances-like pollen, dust mites, or certain foods-as threats. Common examples include hay fever, eczema, asthma, and food allergies. When exposed to an allergen, the immune system releases histamine a chemical that causes itching, swelling, and increased mucus production, leading to the classic symptoms you recognize.
Understanding Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome is a functional gastrointestinal disorder characterized by chronic abdominal pain, bloating, and irregular bowel habits-diarrhea, constipation, or a mix of both. Unlike inflammatory bowel disease, IBS doesn’t cause visible damage to the gut lining, which makes diagnosis rely heavily on symptom patterns and exclusion of other conditions.
Why Researchers See a Connection
Several epidemiological studies published between 2018 and 2024 report that people with allergic disorders are up to 2.5 times more likely to develop IBS. A 2023 meta‑analysis of 27 cohort studies, for example, found a pooled odds ratio of 1.89, indicating a robust association across different age groups and regions.
The link isn’t just statistical; there are plausible biological pathways that tie the two together.
Biological Mechanisms Linking the Two Conditions
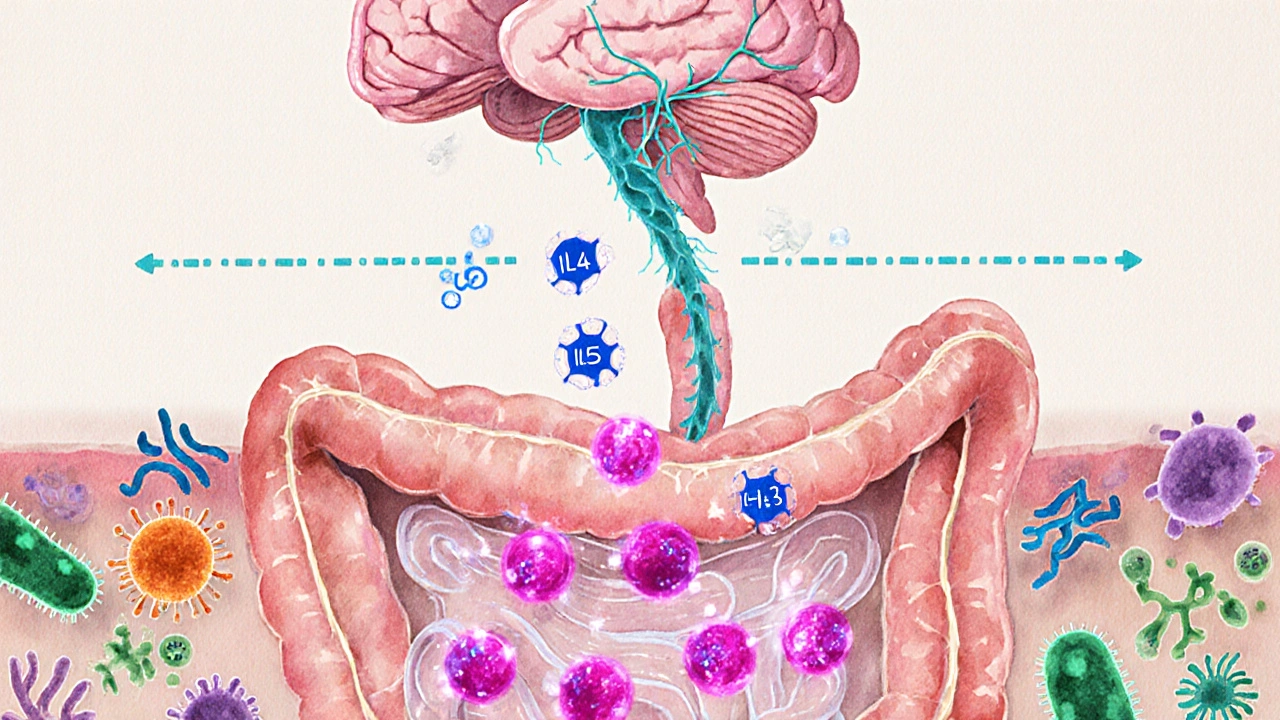
- Immune system activation: When allergens trigger the release of cytokines signaling proteins like IL‑4, IL‑5, and IL‑13 that drive inflammation, they can also affect the gut’s immune environment, leading to heightened sensitivity.
- Gut‑brain axis: Chronic allergic inflammation can alter the gut‑brain axis the bidirectional communication network between the central nervous system and the gastrointestinal tract. This disruption often manifests as IBS‑type symptoms.
- Mast cell involvement: Mast cells-key players in allergic reactions-are abundant in the intestinal wall. Their degranulation releases mediators that increase intestinal permeability, a condition sometimes called "leaky gut," which is a known trigger for IBS.
- Microbiome shifts: Allergic individuals frequently show reduced diversity in the gut microbiome the community of bacteria, fungi, and viruses living inside the intestines. Dysbiosis can impair short‑chain fatty acid production, weakening gut barrier function and fueling IBS symptoms.
- Histamine intolerance: Some people with food allergies also have impaired ability to break down histamine, leading to excess levels that can cause abdominal pain, diarrhea, and bloating-classic IBS signs.
Overlapping Symptoms: What to Watch For
| Symptom | Typical Allergic Trigger | IBS Manifestation |
|---|---|---|
| Abdominal pain | Food allergens (e.g., shellfish, nuts) | Cramping that improves after bowel movement |
| Bloating | Airborne allergens causing sinus drainage | Visible distension, often after meals |
| Diarrhea | Histamine release from mast cells | Loose, urgent stools |
| Constipation | Low‑grade inflammation slowing gut motility | Hard, infrequent stools |
Because these manifestations can arise from unrelated causes, doctors often use a detailed history and, if needed, allergy testing (skin prick or specific IgE) alongside Rome IV criteria for IBS.
Managing Both Conditions Simultaneously
- Identify and eliminate triggers: Work with an allergist to pinpoint specific foods or environmental allergens. Once known, keep a food‑symptom diary to see if IBS flare‑ups correlate.
- Targeted medication: Antihistamines (e.g., cetirizine) can reduce both allergy and histamine‑related gut symptoms. For IBS, antispasmodics or low‑dose tricyclic antidepressants may help.
- Probiotic supplementation: Certain strains such as Lactobacillus rhamnosus have demonstrated benefits in reducing allergic inflammation and improving IBS symptoms. A daily dose of 10‑20billion CFU is a common recommendation.
- Dietary approaches: The low‑FODMAP diet can alleviate IBS pain, while an elimination diet (removing dairy, wheat, soy) can uncover hidden food allergens.
- Stress management: Since stress amplifies both mast cell activity and gut‑brain signaling, techniques like mindfulness, yoga, or CBT are valuable adjuncts.

Practical Lifestyle Tips
- Keep windows closed during high pollen seasons; use HEPA filters to reduce airborne allergen exposure.
- Stay hydrated-water helps flush excess histamine and supports regular bowel movements.
- Prioritize sleep; poor rest can increase cortisol, which in turn worsens gut inflammation.
- Track meals with a simple app, noting timing of symptoms to spot patterns faster.
- Consider a daily omega‑3 supplement rich in EPA/DHA, known to modulate immune response if you have both conditions.
When to Seek Professional Help
If you notice any of the following, schedule an appointment with a gastroenterologist or allergist promptly:
- Sudden weight loss or anemia
- Blood in stool or black, tarry stools
- Severe, unrelenting abdominal pain
- Difficulty breathing or swelling of lips/tongue after eating
- Symptoms that persist despite eliminating known triggers
Early diagnosis not only improves quality of life but can also prevent long‑term complications such as chronic inflammation or nutrient deficiencies.
Frequently Asked Questions
Can an allergy cause IBS?
Allergies can trigger immune and histamine responses that affect gut motility and sensitivity, leading to IBS‑like symptoms. While not every allergic person develops IBS, the risk is notably higher.
Is the low‑FODMAP diet safe for people with food allergies?
Yes, but it should be done under dietitian supervision. The diet eliminates specific fermentable carbs but doesn’t address allergenic proteins, so you may need a separate elimination plan for true food allergies.
Do antihistamines help with IBS pain?
For some patients, especially those with histamine intolerance, non‑sedating antihistamines can reduce abdominal cramping and diarrhea. They’re most effective when combined with other IBS‑targeted therapies.
What role does the gut microbiome play?
A balanced microbiome supports gut barrier integrity and modulates immune responses. Dysbiosis-common in both allergic individuals and IBS patients-can amplify inflammation and symptom severity.
Should I see an allergist, a gastroenterologist, or both?
Starting with an allergist makes sense if you have clear allergy triggers. If gut symptoms dominate or persist after allergy management, a gastroenterologist can evaluate IBS and coordinate care with the allergist.

Taryn Esses
October 5, 2025 AT 18:33Interesting read on the allergy‑IBS link.
Albert Lopez
October 8, 2025 AT 04:00The mechanistic rationale linking atopic pathology to visceral hypersensitivity is well‑documented in peer‑reviewed literature. Cytokine cascades such as IL‑4 and IL‑13 modulate enteric neuronal excitability, thereby predisposing susceptible hosts to IBS‑type symptomatology. Epidemiological cohorts consistently report an odds ratio approaching two for individuals with diagnosed allergies. Nonetheless, correlation does not equate to causality; confounding variables including diet, stress, and microbiome composition warrant rigorous multivariate adjustment. Clinicians should therefore integrate allergy testing into IBS work‑ups only when patient history substantiates a plausible immunologic trigger.
Halle Redick
October 10, 2025 AT 13:43Wow, this article really ties together two things I always thought were separate. If you’ve got hay fever or eczema and you notice belly pain after a meal, it might not just be “bad stomach”. Keeping a simple food‑symptom journal can reveal patterns you’d otherwise miss. Hitting a low‑FODMAP plan while also steering clear of known allergens often gives a double boost. And don’t forget to breathe – mindfulness and a short walk after eating can calm both your immune system and your gut. You’ve got a toolbox here, so experiment and find what clicks for you. Good luck on the journey to feeling better!
Erica Harrington
October 12, 2025 AT 23:26Let’s break this down into doable steps so it doesn’t feel overwhelming. First, schedule a quick visit with an allergist to pinpoint any specific food or environmental triggers. Second, start a daily log noting everything you eat and any gut symptoms that follow – consistency is key. Third, trial a low‑FODMAP diet for two weeks while you’re still testing allergens; many people see relief on both fronts. Fourth, add a probiotic like Lactobacillus rhamnosus to support gut barrier health. Finally, incorporate a few minutes of meditation or gentle yoga each day to ease stress‑related flare‑ups. You’ve got all the tools, now just pick one and get moving!
Patricia Mombourquette
October 15, 2025 AT 09:10Allergy IBS link real It's not a myth. More research needed but data looks solid
karl lewis
October 17, 2025 AT 18:53Esteemed colleagues, it is incumbent upon us to acknowledge the bidirectional communication between the immune and enteric systems as a cornerstone of contemporary gastroenterology. The extant corpus of randomized trials underscores the therapeutic merit of antihistamines in attenuating histamine‑mediated dysmotility. Moreover, judicious application of low‑FODMAP protocols remains a mainstay in symptomatic management. I would therefore advocate for an interdisciplinary clinic where allergists and gastroenterologists jointly evaluate complex cases. 😊
Amy Martinez
October 20, 2025 AT 04:36Reading this felt like unlocking a secret level in the game of health-so many hidden connections! The way mast cells can throw a wild party in the gut, spilling histamine like confetti, explains those sudden belly rumbles after pollen season. I’ve personally found that swapping out a bland diet for a vibrant, probiotic‑rich plan made my IBS symptoms melt away like ice in sunshine. And the tip about omega‑3s? Pure gold-those little fish‑oil warriors calm inflammation like a gentle tide. Keep sharing these gems; they’re a lifeline for anyone stumbling through the allergy‑IBS maze.
Josh Grabenstein
October 22, 2025 AT 14:20They don’t want you to know that the pharma industry pushes meds instead of addressing the real trigger hidden in your own environment. Your kitchen air, the pollen that sneaks through the windows, can set off mast cells and mess with your gut without you ever suspecting it. Cutting out the obvious allergens and watching the gut react is the only true experiment they won’t fund. Trust the data they hide, not the headlines they promote. Stay curious, stay skeptical.
Nidhi Jaiswal
October 25, 2025 AT 00:03Good info on how allergies can affect the gut. Try to keep a diary of foods and symptoms. It helps doctors find the cause faster.
Sunil Sharma
October 27, 2025 AT 08:46Hey folks, just wanted to add a friendly reminder that you don’t have to tackle this alone. Pair up with a dietitian who knows about both low‑FODMAP and food allergies – they can craft a plan that respects both needs. Also, involve a trusted friend or family member in your food‑logging routine; accountability makes a big difference. And remember, small sustainable changes beat drastic diets that you can’t keep up with. You’ve got a supportive community right here.
Jenn Zee
October 29, 2025 AT 18:30It is quite astonishing how often the medical literature glosses over the profound implications of immunologic dysregulation on functional gastrointestinal disorders, especially when the data are as compelling as the meta‑analyses cited in this piece. First, the authors correctly highlight that cytokine‑mediated inflammation can sensitize enteric neurons, yet they stop short of exploring the downstream effects on visceral hyperalgesia in a mechanistic sense. Second, while the statistical association of a 2.5‑fold increased risk is noteworthy, the narrative fails to contextualize this figure within the heterogeneity of study populations and diagnostic criteria for both allergy and IBS. Third, the recommendation to pursue simultaneous allergist and gastroenterologist consultations is sound, but it neglects the practical barriers many patients face, such as insurance limitations and geographic access. Fourth, the emphasis on low‑FODMAP diets as a universal remedy disregards the fact that such diets can inadvertently exacerbate nutritional deficiencies if not properly supervised. Fifth, the suggestion to incorporate probiotics, particularly Lactobacillus rhamnosus, is intriguing, yet the cited studies often involve small sample sizes and short follow‑up periods, which calls for cautious interpretation. Sixth, the article mentions histamine intolerance but does not delve into the enzymatic deficiencies-namely DAO deficiency-that underlie this condition, leaving readers without a clear diagnostic pathway. Seventh, the exploration of mast cell activation syndrome is cursory at best, overlooking cutting‑edge biomarkers that could refine patient selection for targeted therapies. Eighth, the discussion of stress management techniques, while valuable, is presented as an afterthought rather than an integrated component of a biopsychosocial model. Ninth, the authors’ reliance on self‑reported symptom questionnaires introduces a level of subjectivity that could be mitigated by incorporating objective measures such as intestinal permeability tests. Tenth, the recommendation to use omega‑3 supplementation is supported by some evidence, but the optimal dosing and formulation remain contentious. Eleventh, the brief mention of environmental controls, such as HEPA filters during pollen season, is a practical tip that deserves greater emphasis given its low cost and high impact. Twelfth, the article’s conclusion, albeit optimistic, borders on overgeneralization by implying that early diagnosis will universally prevent long‑term complications, a claim that requires longitudinal data to substantiate. Thirteenth, the inclusion of a concise FAQ section is helpful, yet the answers could be expanded to address common misconceptions about cross‑reactivity between food allergens and gut flora. Fourteenth, the overall tone of the piece is reassuring, which is beneficial for patient morale, but it should be balanced with a realistic appraisal of treatment timelines and potential setbacks. Finally, while the integration of interactive risk assessment tools is a commendable innovation, the authors must ensure that such tools are validated across diverse populations to avoid inadvertently widening health disparities. In sum, the article provides a solid foundation, but a more nuanced, evidence‑rich, and patient‑centred approach would elevate it from a useful overview to a truly actionable roadmap for individuals navigating the intertwined realms of allergy and IBS.
don hammond
November 1, 2025 AT 04:13Wow, thanks for the PhD thesis in a Reddit comment – really needed that extra 2,000 words 😏📚
Ben Rudolph
November 3, 2025 AT 13:56Sure, but at the end of the day the practical steps matter more than the academic flair.
Charlotte Shurley
November 5, 2025 AT 17:30Totally agree, brief and to the point works wonders for quick reads.