Managing bipolar disorder isn’t about finding one magic pill. It’s about balancing two powerful classes of medication-mood stabilizers and antipsychotics-while dealing with side effects that can feel just as overwhelming as the mood swings themselves. For many people, the goal isn’t just to stop manic or depressive episodes. It’s to live without constant fear of the next crash, without losing weight, energy, or mental clarity to the drugs meant to save them.
Why These Medications Are the Foundation
Lithium, first approved in 1970, is still the most studied and trusted mood stabilizer. It doesn’t just calm mania-it reduces suicide risk by 80% compared to no treatment. That’s not a small number. It’s life-saving. But lithium isn’t simple. You need regular blood tests. Levels must stay between 0.6 and 1.0 mmol/L. Go above 1.2, and you risk toxicity-slurred speech, shaking, even seizures. Most people on lithium drink liters of water a day because it makes you urinate constantly. Weight gain is common, and so are hand tremors. But for many, it’s the only thing that stops the cycle. Antipsychotics like quetiapine (Seroquel) and olanzapine came into the picture later, but they’ve become just as important. Quetiapine was approved for bipolar depression in 2006. It works faster than lithium-some people feel better in a week. But it comes with trade-offs. Around 60-70% of users feel drowsy. Weight gain is almost guaranteed. One study showed people gained an average of 4.6kg in just six weeks. That’s not just inconvenient-it increases diabetes risk by 20-30% with some drugs.How They Compare: Lithium vs. Quetiapine vs. Lamotrigine
Not all mood stabilizers are the same. Here’s how the most common ones stack up:| Medication | Best For | Typical Starting Dose | Key Side Effects | Response Rate |
|---|---|---|---|---|
| Lithium | Mania and long-term prevention | 300mg daily | Thirst, tremors, weight gain, kidney/thyroid issues | 47% relapse prevention (12 months) |
| Quetiapine | Depression and acute mania | 50mg nightly | Drowsiness, weight gain, metabolic syndrome | 50.3% for depression |
| Lamotrigine | Depression (minimal mania risk) | 25mg weekly, slowly increased | Severe rash (10% risk), insomnia | 47% for depression |
| Valproate | Mania (especially rapid cycling) | 500mg daily | Weight gain, liver stress, birth defects | 60% for acute mania |
Lamotrigine is the quiet hero for depression. It doesn’t cause much weight gain, and it’s gentle on metabolism. But if you’re not careful with the dose ramp-up, you can get a life-threatening rash. That’s why doctors start at 25mg a week and take months to reach therapeutic levels. It’s slow, but it’s safe-if you follow the plan.
Combination Therapy: When Two Drugs Are Better Than One
Many people don’t respond to just one medication. That’s where combinations come in. Adding an antipsychotic like aripiprazole to lithium or valproate can push response rates up to 70% in treatment-resistant cases. But here’s the catch: side effects pile up. Weight gain, drowsiness, metabolic issues-they don’t cancel out. They multiply. One study found side effect burden jumped by 25-30% with combo therapy. That’s why doctors don’t jump to combinations right away. They try one drug, give it time, adjust the dose, then add another only if needed. It’s not about throwing everything at the wall. It’s about precision.Why People Stop Taking Their Medication
About 40% of people with bipolar disorder stop their meds within a year. That’s not because they’re noncompliant. It’s because the side effects are brutal. A 2022 survey by NAMI found:- 78% stopped or reduced meds due to weight gain
- 65% said they felt mentally foggy or slow
- 52% reported sexual dysfunction

Monitoring: What Your Doctor Should Be Checking
Medication management isn’t a one-time prescription. It’s ongoing monitoring. For lithium, you need blood tests weekly at first, then every 2-3 months. Your kidney and thyroid function must be checked at least once a year. For antipsychotics, you need regular checks on:- Weight and waist size (over 40 inches for men, 35 for women = metabolic risk)
- Fasting blood sugar
- Lipid levels (cholesterol and triglycerides)
Drug Interactions You Can’t Ignore
Lithium and ibuprofen? That’s a bad mix. NSAIDs like Advil or Aleve can spike lithium levels by 25-60%, pushing you into toxicity territory. Even common antibiotics like amoxicillin can interfere. Antipsychotics interact with over 40 other drugs-some heart medications, some antidepressants, even grapefruit juice. That’s why you need one doctor who knows your full list of meds. Not just your psychiatrist. Your primary care provider, your dentist, your pharmacist. Everyone needs to be on the same page. A simple OTC cold medicine could trigger a manic episode or a seizure.What’s New in 2025
The field is changing. In 2023, the FDA approved lumateperone (Caplyta) for bipolar depression. Unlike quetiapine, it causes only 0.8kg of weight gain in six weeks-almost none compared to the 3.5kg seen with older drugs. Long-acting injectables like Abilify Maintena mean you only need one shot a month. No daily pills. No forgetting. That’s huge for people who struggle with adherence. Genetic testing is starting to show promise. About 40% of bipolar meds are metabolized by enzymes (CYP2D6, CYP2C19) that vary wildly between people. A simple blood test can now tell you if you’re a fast or slow metabolizer. That helps doctors pick the right drug and dose from the start. It’s not standard yet-but it’s coming fast.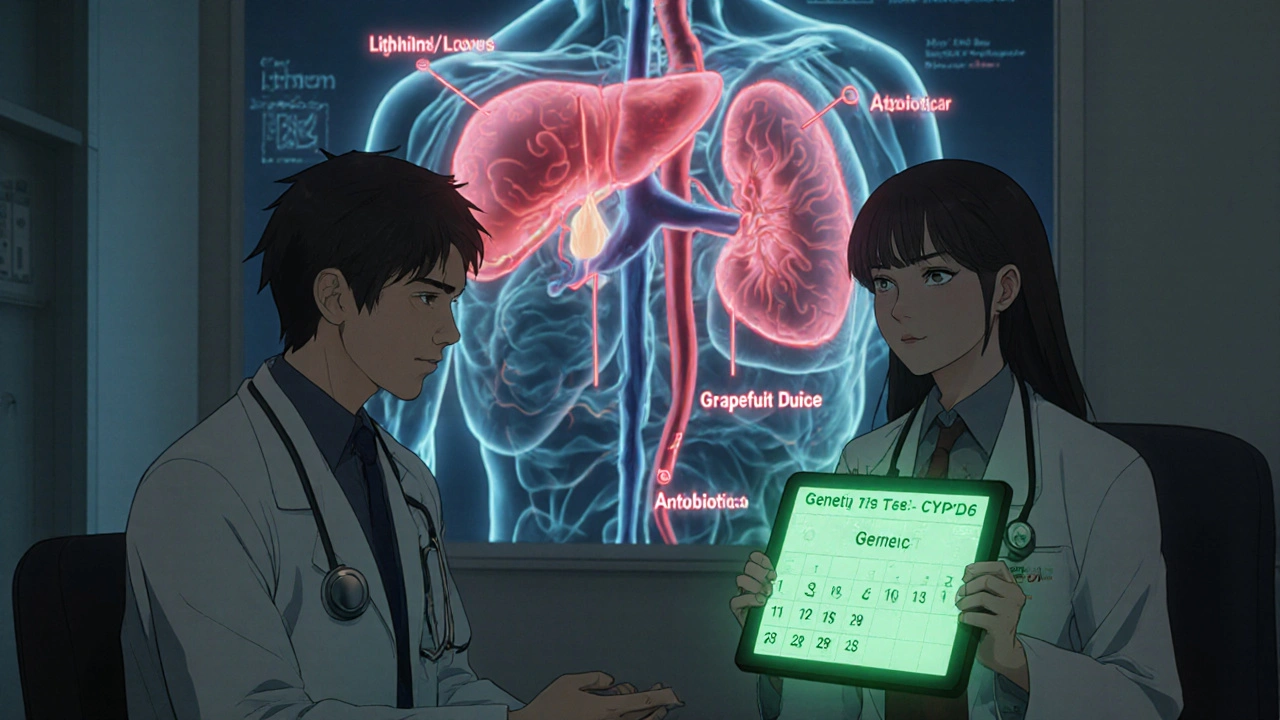
What Works for One Person Might Not Work for Another
There’s no universal formula. One person thrives on lithium. Another can’t tolerate even a low dose. One finds quetiapine life-changing. Another can’t sleep, can’t function, and gains 30 pounds. The key is patience and communication. Tell your doctor if you’re tired all the time. If your sex drive vanished. If you’re gaining weight despite eating the same. If you’re scared to take the pill because of how it made you feel last time. And don’t quit cold turkey. Stopping antipsychotics suddenly can trigger rebound mania. Stopping lithium too fast can bring back depression with a vengeance. Tapering matters.What to Ask Your Doctor
If you’re on these meds-or thinking about starting them-ask:- Which medication are you starting me on, and why?
- What side effects should I expect in the first month?
- How often will I need blood tests?
- What signs of toxicity or serious reactions should I watch for?
- Are there cheaper generic options?
- Can we try a lower dose first and build up slowly?
Final Reality Check
Only 35% of people with bipolar disorder reach full remission. Six in ten still deal with serious side effects. These drugs aren’t perfect. But for millions, they’re the difference between living and surviving. The goal isn’t to feel perfectly normal. It’s to feel stable enough to get up, go to work, hold a conversation, laugh with a friend. To not wake up every day wondering if today’s the day you won’t make it. Medication is one part of the puzzle. Therapy, sleep, routine, support-those matter too. But without the right meds, the rest is often impossible.Can mood stabilizers cause depression?
Mood stabilizers like lithium and lamotrigine are designed to prevent both mania and depression. But some people report feeling emotionally flat or lethargic, especially at higher doses. This isn’t true depression, but it can feel like it. If you feel numb, apathetic, or unable to enjoy things, talk to your doctor. It may be a dose issue, not a treatment failure.
Is it safe to take antidepressants with bipolar disorder?
Antidepressants can be risky for bipolar disorder. They can trigger mania or rapid cycling in 10-25% of cases. If used at all, they should only be taken with a mood stabilizer or antipsychotic. SSRIs like fluoxetine are sometimes used for severe depression, but only under close supervision. Many experts recommend avoiding them unless absolutely necessary.
How long does it take for mood stabilizers to work?
Lithium and valproate usually take 1-3 weeks to show full effect for mania. Lamotrigine takes much longer-up to 8-12 weeks for depression. Antipsychotics like quetiapine can work in as little as 7 days. Patience is key, but if you see no change after 6 weeks, it’s time to reassess with your doctor.
Can I drink alcohol while on these medications?
Alcohol can worsen drowsiness from antipsychotics and increase the risk of lithium toxicity. It can also trigger mood episodes. Most doctors advise avoiding alcohol entirely. Even one drink can throw off your balance-emotionally and physically.
What if I can’t afford my medication?
Lithium carbonate costs as little as $4-$40 a month as a generic. Many antipsychotics are available as generics too. If you’re paying over $200/month for a brand-name drug, ask your doctor about alternatives. Pharmaceutical companies often have patient assistance programs. Your pharmacy can help you apply.

mike tallent
November 18, 2025 AT 03:42Been on lithium for 8 years. Tremors? Yeah. Thirst? Constant. But I held my job, kept my kids, and didn’t end up in the ER once. Worth every sip of water. 💪💧
Deepali Singh
November 18, 2025 AT 21:22The data here is statistically sound but ignores the real human cost: loss of identity. When your emotional range is reduced to ‘stable’ and ‘not suicidal,’ you’re not living-you’re surviving in grayscale. The paper doesn’t mention grief for the person you were before meds.
Joyce Genon
November 19, 2025 AT 15:27Let’s be real-this whole article reads like a pharma brochure dressed up as patient advocacy. Sure, lithium reduces suicide risk, but so does having a supportive family, therapy, and not being forced into a medical model that treats your brain like a malfunctioning toaster. And don’t get me started on how ‘metabolic syndrome’ is just a fancy way of saying ‘you gained weight and now you’re a liability.’ The real problem? Doctors don’t listen. They prescribe, monitor, and move on. Meanwhile, you’re left Googling ‘can lamotrigine make you cry for no reason’ at 3 a.m.
Julie Roe
November 19, 2025 AT 20:49I’ve been on lamotrigine for 5 years. Slow ramp-up? Yes. Scary rash? I was terrified. But I finally feel like me again-not numb, not zombified, not gaining 20 pounds. I still have bad days, but they’re *my* bad days, not drug-induced fog. If you’re scared to start, start low. If your doctor won’t go slow, find a new one. You deserve to feel human, not just stable.
George Gaitara
November 20, 2025 AT 18:56Why are we still using 1970s drugs? We have AI-driven neuroimaging now. We can map serotonin pathways in real time. Why are people still getting blood drawn every 3 months like we’re in 1995? This is medical malpractice disguised as ‘standard care.’ Someone’s getting paid to keep this system alive.
jalyssa chea
November 22, 2025 AT 03:47im on serequel and its hell but i cant stop because i almost killed myself last year and now i just feel like a blob who cant even enjoy pizza anymore
Peter Stephen .O
November 24, 2025 AT 03:22Y’all need to hear this: meds aren’t the enemy, silence is. If you’re tired, say it. If you’re gaining weight, say it. If your libido’s gone, scream it into the void. Doctors can’t fix what they don’t know. And yes, asking for a lower dose or a different med? That’s not weakness-that’s warrior energy. 🚀
Andrew Cairney
November 24, 2025 AT 14:37Did you know the FDA approved lumateperone because Big Pharma needed a ‘clean’ antipsychotic to replace olanzapine? The weight gain numbers? Manipulated. The trials? Excluded people with diabetes. And the injectables? They’re not for adherence-they’re for control. You think you’re choosing treatment? You’re being managed.
Jennifer Howard
November 24, 2025 AT 20:35It is imperative to note that the author, while well-intentioned, exhibits a dangerous romanticization of pharmacological intervention. The reliance on lithium, a compound with documented nephrotoxic and thyrotoxic potential, constitutes a systemic failure of modern psychiatry to prioritize holistic, non-pharmacological modalities. One cannot ethically endorse a treatment paradigm that reduces human complexity to serum concentrations and metabolic panels. The true cure lies in spiritual alignment, circadian regulation, and elimination of processed sugars-none of which are mentioned herein.
Rob Goldstein
November 25, 2025 AT 14:41For anyone reading this and feeling overwhelmed: you’re not alone. The CYP2D6 poor metabolizer phenotype is way more common than people think-especially in East Asian and Indigenous populations. If you’re on quetiapine and feel like a zombie, it might not be ‘you’-it might be your liver. Ask for pharmacogenetic testing. It’s not sci-fi-it’s in your insurance plan. And if your doc says ‘we don’t do that here,’ ask for a referral. You deserve precision, not trial-and-error.
Sylvia Clarke
November 26, 2025 AT 00:18Oh, so now we’re supposed to be grateful that lithium lets us ‘survive’ instead of ‘live’? How poetic. We’ve turned mental health into a survivalist sport where the prize is not dying-and we call that progress. Meanwhile, the real tragedy isn’t the side effects-it’s that we’ve normalized the idea that feeling like a human being is a luxury reserved for the neurotypical. You want to know why people stop meds? It’s not because they’re lazy. It’s because they’re tired of being told to be grateful for a life that feels like a slow-motion funeral.
Abdul Mubeen
November 27, 2025 AT 14:46Who funds this research? Who owns the patents on lithium? Who benefits from lifelong blood tests? The pharmaceutical industry has spent decades turning bipolar disorder into a profitable chronic condition. The ‘80% suicide reduction’ statistic? Correlation, not causation. Lithium is a byproduct of nuclear waste processing. Coincidence? I think not. The real treatment? Get off the grid. Eat clean. Meditate. Stop trusting doctors who get paid per script.
Gary Lam
November 28, 2025 AT 20:15As a Thai-American, I’ve seen how Western medicine treats bipolar like a broken machine. In my culture, we talk about ‘balancing energy’-not dosing chemicals. My grandma used turmeric, sleep schedules, and family meals. I’m not saying ditch the meds-but don’t forget the roots. Maybe the ‘side effects’ aren’t the problem. Maybe the whole damn system is.
John Wayne
November 30, 2025 AT 06:01It’s amusing how this piece frames medication compliance as a moral victory. The subtext is clear: if you’re not taking lithium, you’re weak. If you’re gaining weight, you lack discipline. The arrogance of this narrative is staggering. Mental illness is not a character flaw. Neither is the decision to prioritize quality of life over longevity.