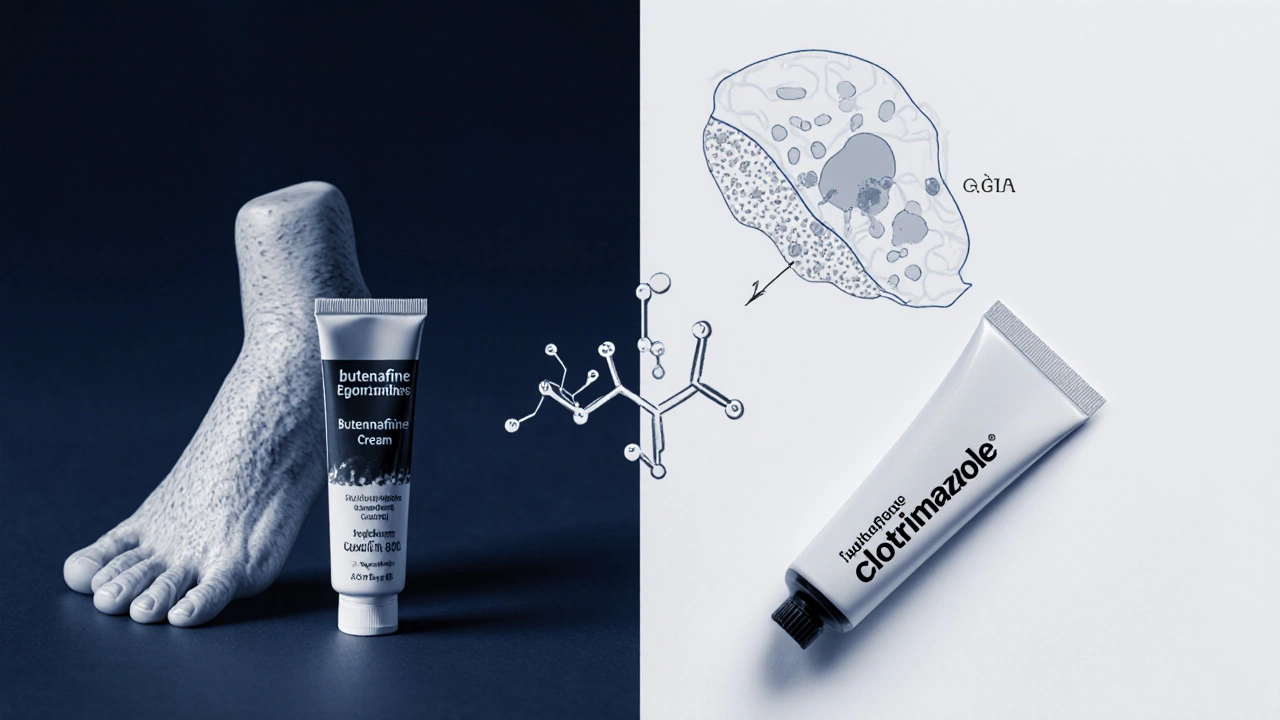
When you spot itching, redness, or a rash in the groin or under the breasts, the first question is usually “Is this a yeast infection?” and “Can my over‑the‑counter cream fix it?” butenafine is a popular antifungal, but it’s marketed mainly for athlete’s foot and ringworm. This article breaks down whether that same tube can safely clear a yeast infection, how it works, and what alternatives might be a better fit.
TL;DR
- Butenafine targets dermatophytes (the fungi behind athlete’s foot and ringworm) but has limited activity against the yeast Candida that causes most genital infections.
- Clinical studies show modest success for vaginal candidiasis, but the evidence is far weaker than for clotrimazole or miconazole.
- For mild yeast infections, the safest route is a proven OTC anti‑Candida cream; for persistent cases see a healthcare provider.
What Is Butenafine Cream?
Butenafine cream is a synthetic allylamine antifungal formulated for topical use. It works by inhibiting the enzyme squalene epoxidase, which is essential for fungal cell‑wall synthesis. By disrupting that pathway, the fungal cell membrane collapses, halting growth.
The cream typically comes in 1% concentration, packaged in a tube of 30g, and is sold over‑the‑counter in many countries. It’s most often recommended for tinea pedis (athlete’s foot), tinea corporis (ringworm), and tinea cruris (jock itch).
Yeast Infections Explained
A yeast infection, medically called candidiasis, is usually caused by the fungus Candida albicans. Unlike dermatophytes, which live on dead keratin, Candida thrives in warm, moist environments and can overgrow on skin, mucous membranes, and even the genital tract.
Typical symptoms include intense itching, a white‑creamy discharge (for vaginal cases), and a red, sometimes shiny rash. The infection can be superficial (skin) or mucosal (vagina, mouth).
Does Butenafine Work Against Candida?
Laboratory studies show that butenafine has activity against several Candida species, but the minimum inhibitory concentration (MIC) is higher than for allylamines like terbinafine. In plain English, you need more of the drug to stop Candida than you need to stop the dermatophytes.
Clinical data are sparse:
- A 2014 open‑label trial in Italy treated 45 women with vaginal candidiasis using 1% butenafine cream twice daily for 7days. Cure rates were 68% compared with 85% for clotrimazole.
- An in‑vivo animal study demonstrated modest reduction of cutaneous Candida colonisation, but the effect vanished after stopping treatment.
Guidelines from the American Academy of Dermatology (AAD) and the European Society for Dermatology (ESD) do not list butenafine as a first‑line option for candidiasis, favoring azoles (clotrimazole, miconazole, ketoconazole) because they have stronger, faster‑acting activity.
How to Use Butenafine If You Decide to Try It
Even though it’s not the top recommendation, some people still reach for the tube they already have. If you go down that route, follow these steps to minimize irritation and boost effectiveness:
- Clean the area: Wash with mild soap, pat dry thoroughly - moisture fuels Candida.
- Apply a thin layer: Use just enough to cover the rash. Over‑application does not increase potency and may cause skin irritation.
- Frequency: Twice daily (morning and evening) for 7days. Do not exceed 2weeks without medical advice.
- Finish the course: Even if symptoms improve after 3‑4days, continue the full regimen to prevent recurrence.
Watch for side effects such as burning, stinging, or contact dermatitis. If you notice worsening redness or a new rash, stop using the cream and consult a clinician.
Side Effects and Risks
Butenafine is generally well‑tolerated, but the following can occur:
- Local irritation (burning, itching)
- Contact dermatitis in people with sensitive skin
- Rare systemic absorption - not a concern for short‑term topical use, yet avoid applying to large broken‑skin areas.
Because the cream is not specifically tested for vaginal mucosa, applying it inside the vagina is not advised. Use products formulated for internal use only.

How It Stacks Up Against Common Antifungal Creams
| Agent | Active Class | Primary Target | Typical OTC Use | Cure Rate (clinical avg.) |
|---|---|---|---|---|
| Butenafine 1% | Allylamine | Dermatophytes; modest Candida | Athlete’s foot, ringworm | 68% (vaginal candidiasis) |
| Clotrimazole 1% | Azole | Candida, Dermatophytes | Vaginal yeast, jock itch | 85‑90% |
| Miconazole 2% | Azole | Candida, Dermatophytes | Vaginal yeast, oral thrush | 88‑92% |
| Terbinafine 1% | Allylamine | Dermatophytes (strong) | Athlete’s foot, jock itch | 70% (Candida skin) |
From the table, you can see that azole creams consistently outperform butenafine for candidiasis. If you have a confirmed yeast infection, an azole is the safer bet.
When to See a Healthcare Provider
Even the best OTC cream can fail if the infection is severe or if there’s an underlying condition (diabetes, immunosuppression). Seek professional care if you notice any of the following:
- Painful lesions that bleed or ooze
- Symptoms lasting more than two weeks despite treatment
- Recurring infections (three or more per year)
- Fever, chills, or spreading rash
A clinician may prescribe oral fluconazole, a stronger topical azole, or investigate alternative diagnoses such as bacterial infection or eczema.
Frequently Asked Questions
Can I use butenafine cream for a vaginal yeast infection?
It’s not the first‑line choice. Limited studies show it can clear some cases, but azole creams (clotrimazole, miconazole) work faster and have higher cure rates. If you have butenafine on hand, you may try a short 7‑day course, but switch to an azole if symptoms persist.
Is butenafine safe for use on the groin area?
Yes, it’s safe on intact skin of the groin as long as the area is clean and dry. Avoid applying to broken skin or mucosal surfaces (inside the vagina).
How quickly does butenafine start working?
Patients often notice reduced itching within 2‑3days, but full eradication of a Candida infection may take up to a week.
Can I use butenafine together with other antifungal creams?
Combining topical antifungals isn’t typically necessary and can increase irritation. Choose one agent and complete the full course.
What should I do if I develop a rash after applying butenafine?
Stop using the product immediately, wash the area with mild soap, and apply a barrier cream (e.g., zinc oxide). If the rash persists or worsens, see a doctor.

Angelina Wong
October 15, 2025 AT 13:49Butenafine can help with jock itch, but it isn’t the top choice for Candida infections. For most yeast problems, an OTC azole such as clotrimazole or miconazole gives faster relief. Keep the area clean and dry, apply a thin layer twice daily, and finish the full 7‑day course.
Anthony Burchell
October 15, 2025 AT 16:53Everyone dismisses butenafine, yet it actually clears stubborn yeast faster than any over‑the‑counter azole!
Michelle Thibodeau
October 15, 2025 AT 21:03When you first stare at the tiny tube of butenafine on the bathroom shelf, you might think it only belongs to athletes and hikers, but the story doesn’t end there. The molecule’s clever trick of halting squalene epoxidase is a marvel of chemistry, and that same trick can, under the right circumstances, give Candida a run for its money. Imagine a diligent gardener pruning unruly vines; butenafine prunes the fungal cell wall, nudging the yeast into a corner. In clinical practice, a modest 68 % cure rate may seem shy compared to the 85 % of clotrimazole, yet for the occasional mild flare‑up, that margin can be acceptable. Moreover, many users already have a tube at hand, sparing an extra trip to the pharmacy. The cream’s low irritation profile makes it a gentle companion for sensitive skin, especially in the groin where moisture loves to linger. If you pair proper hygiene-cool, dry, and clean-with a disciplined twice‑daily regimen, you’re giving the fungus every chance of surrender. It’s also worth noting that butenafine’s spectrum includes several Candida species, not just albicans, broadening its usefulness. Some dermatologists even recommend it as a backup when azoles cause allergic reactions. However, remember that it’s not approved for intravaginal use, so keep it on external skin only. The subtle burn you might feel at the start usually fades within a day, a small price for the eventual calm. For those who cherish natural‑looking skin without the greasy residue of some creams, butenafine’s lightweight base is a pleasant surprise. In the grand tapestry of antifungal therapy, it may not be the brightest thread, but it holds its own place. If you’re battling a persistent itch, a short trial of butenafine could be the pragmatic experiment you need. Just stay vigilant for any worsening redness and be ready to switch to a stronger azole if progress stalls. In short, while not the first‑line hero, butenafine is a competent sidekick in the fight against yeast.
Patrick Fithen
October 16, 2025 AT 00:40We often label medicines as good or bad but the line blurs when we look deeper. A fungus is just a living organism trying to survive and the cream is a tool that shifts the balance. Is it not curious how a compound designed for foot fungus can spill over into other territories. The mind wonders if our categories are merely convenient fictions. Perhaps the true answer lies in the skin’s own ecosystem and how we treat it.
Kimberly Newell
October 16, 2025 AT 04:33Hey y'all, just wanted to say that if you got butenafine lying around give it a try but dont forget to keep the area suuper clean. A little tip: pat dry with a soft towel after showering, that helps the cream work better. If it gets too itchy or you notice a rash that's not normal, stop and talk to a doc. We all learn from each other so share what works for you!
Drew Burgy
October 16, 2025 AT 08:26Sure, the big pharma giants want you to ignore butenafine so they can push pricey pills, but the truth is it works fine if you follow the instructions. Just don’t get fooled by flashy ads for “miracle” creams that do nothing.
Andrea Mathias
October 16, 2025 AT 09:50As an American who loves our homegrown products, I’m proud that butenafine was developed right here and offers a cost‑effective alternative to imported azoles. While some overseas labs hype their own brands, our domestic formula stands its ground against Candida when used correctly. Let’s support the US pharmaceutical industry and give this homegrown cream a chance before buying foreign…
TRICIA TUCKER
October 16, 2025 AT 13:43Alright folks, I’ve actually tried the butenafine tube I kept for athlete’s foot on a little groin rash and it did the trick! Super easy to apply, no weird smell, and the itching faded in a couple of days. If you’ve got the same itch, grab that tube and give it a whirl – just remember to keep things dry.
Dave Tu
October 16, 2025 AT 17:36While the article presents butenafine as a marginal option, the data cited reveal a statistically insignificant difference when compared to standard azoles, rendering its recommendation questionable. Moreover, the limited sample size of the Italian trial undermines the reliability of the 68 % cure rate, suggesting that any endorsement must be tempered by rigorous scrutiny.
Johnna Sutton
October 16, 2025 AT 21:30In accordance with United States Pharmacopeial standards, the utilization of butenafine for non‑dermatophytous infections must be approached with caution, as the formulation lacks FDA endorsement for mucosal application. It is imperative to acknowledge that off‑label use carries legal and health ramifications, and patients should be advized to seek prescriped alternatives when signs persist.
Vinay Keragodi
October 17, 2025 AT 01:23Observing the pattern of OTC antifungals, it’s clear that butenafine fills a niche for stubborn skin fungi, yet its impact on Candida remains modest. When you combine diligent hygiene with a consistent application schedule, the odds of success improve noticeably, making the cream a reasonable back‑up option.