Cephalosporin Cross-Reactivity Calculator
This calculator helps you understand your actual risk of allergic reaction when considering cephalosporin antibiotics after a penicillin allergy.
Based on the latest medical research, cross-reactivity depends on:
- your specific type of penicillin reaction
- the generation of cephalosporin
- side chain similarity
Your Personalized Risk Assessment
Why Most People with Penicillin Allergy Can Safely Take Cephalosporins
If you’ve ever been told you can’t take cephalosporins because you’re allergic to penicillin, you’ve probably heard the 10% rule. That number-10%-has been repeated for decades in medical textbooks, hospital protocols, and even on drug labels. But here’s the truth: that number is outdated, misleading, and costing patients better care.
Back in the 1960s and 70s, researchers found that about 10% of people with penicillin allergies also reacted to cephalosporins. Sounds scary, right? But those early studies were flawed. The cephalosporins made back then weren’t pure. They were contaminated with tiny traces of penicillin because of how they were grown in the same mold cultures. So when patients reacted, it wasn’t because the cephalosporin structure triggered their allergy-it was because they were accidentally getting penicillin.
Today, manufacturing is clean. Modern cephalosporins contain no penicillin residue. And when you look at the real data from studies done since the 1990s, the actual cross-reactivity rate is closer to 2-5% for first- and second-generation cephalosporins-and less than 1% for third- and fourth-generation ones like ceftriaxone and cefepime.
The Real Reason Cross-Reactivity Happens (It’s Not What You Think)
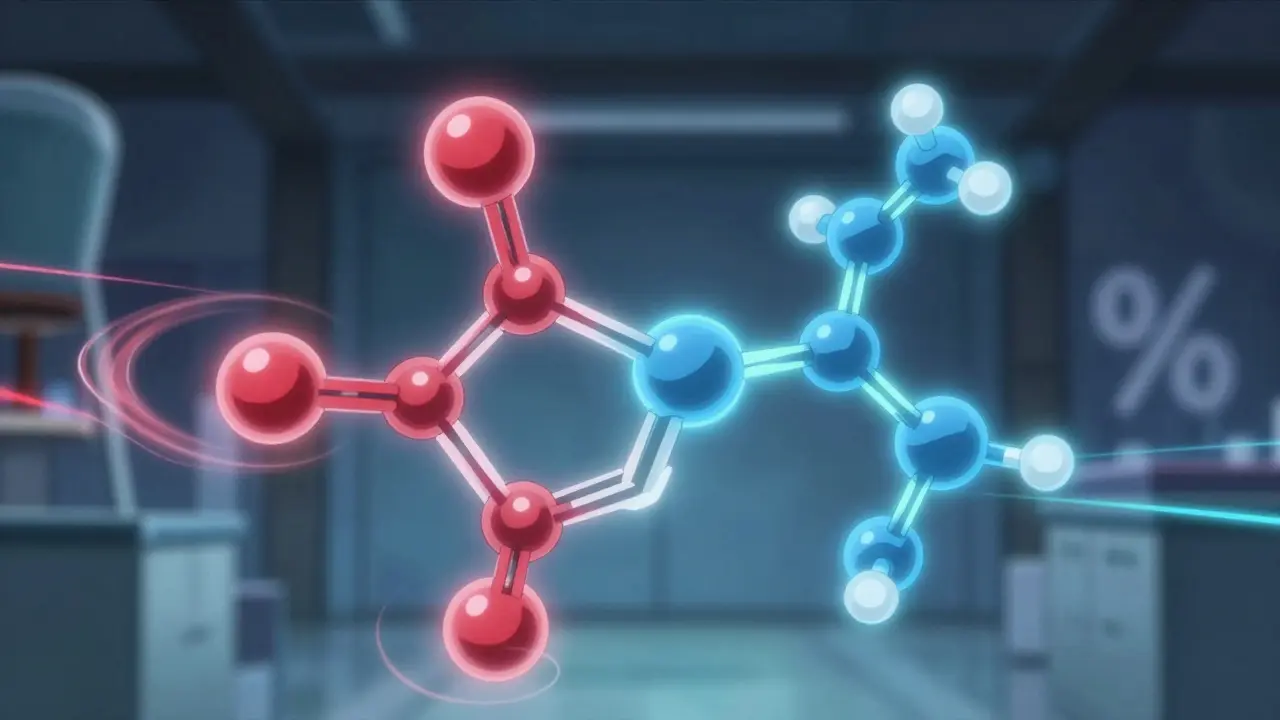
Most people assume cross-reactivity happens because penicillins and cephalosporins both have a beta-lactam ring. That’s the four-membered ring structure that gives these antibiotics their power. But here’s the twist: your immune system doesn’t really care about the ring.
What it reacts to is the side chain-the chemical group sticking off the main structure. Think of it like this: if two drugs have the same side chain, your body might confuse them. But if the side chains look different, even if the core ring is the same, your immune system usually doesn’t care.
Studies show that 42% to 92% of penicillin allergic reactions are tied to the side chain, not the beta-lactam ring. That’s why amoxicillin and ampicillin-two penicillins with nearly identical side chains-often cross-react with each other. But ceftriaxone, a third-generation cephalosporin, has a side chain so different from penicillin that your immune system treats it like a completely new molecule.
This is why doctors now look at side-chain similarity when deciding if a cephalosporin is safe. If you’re allergic to amoxicillin, you might still be able to take ceftriaxone. But you’d want to avoid cefaclor, which shares a similar side chain with amoxicillin. It’s not about the class-it’s about the molecular fingerprint.
Generations Matter: Which Cephalosporins Are Riskiest?
Cephalosporins are grouped into five generations based on when they were developed and what bacteria they kill. But they also matter because of how their side chains changed over time.
- First-generation (cefazolin, cephalexin): Closest in structure to penicillin. Cross-reactivity risk: 1-8%.
- Second-generation (cefuroxime, cefaclor): Slightly more different. Risk: 1-5%.
- Third-generation (ceftriaxone, cefotaxime, cefixime): Very different side chains. Risk: less than 1%.
- Fourth-generation (cefepime): Even more distinct. Risk: less than 1%.
- Fifth-generation (ceftaroline, ceftolozane/tazobactam): Newer, unique structures. No clear data yet, but early signs suggest low risk.
Here’s what this means in practice: if you need an antibiotic for a urinary tract infection or pneumonia and you have a penicillin allergy, ceftriaxone is often safer than clindamycin or azithromycin-which come with higher risks of C. diff infection or antibiotic resistance.
And here’s the kicker: many patients with penicillin allergies have never had a true IgE-mediated reaction. They might’ve had a rash as a kid, or stomach upset, or thought they were allergic because a doctor said so. But true anaphylaxis-swelling, trouble breathing, low blood pressure-is rare. Studies show that among people who say they’re allergic to penicillin, 90-95% can safely take it after proper testing.
What Counts as a Real Penicillin Allergy?
Not every bad reaction is an allergy. There’s a big difference between:
- IgE-mediated allergy: Hives, swelling, wheezing, anaphylaxis. This is a true immune response, usually happening within minutes to hours.
- Delayed rash: A non-itchy, flat rash that appears days after starting the drug. Often not immune-mediated-could be viral or drug-related irritation.
- GI upset: Nausea, diarrhea. That’s not an allergy. That’s a side effect.
The CDC and major allergy societies say that if you’ve never had a severe reaction (anaphylaxis, hives, throat swelling) in the last 10 years, you can likely take third- and fourth-generation cephalosporins without testing. Even if you had a rash as a child, it probably wasn’t a true allergy. Most kids outgrow penicillin allergies by adulthood.
But here’s where things get tricky: some people have had anaphylaxis to penicillin. In those cases, doctors are still cautious. But even then, the risk isn’t 10%. It’s closer to 0.5-1% for ceftriaxone. And if the side chain is very different, the risk drops even more.
Why So Many Doctors Still Get It Wrong
Despite decades of new research, many providers still believe the 10% myth. A 2020 survey found that 80-90% of clinicians still think all cephalosporins carry a 10% cross-reactivity risk. Why?
- Drug labels haven’t changed. The FDA still warns of 10% cross-reactivity on cephalosporin packaging, even though the evidence says otherwise.
- Medical education lags. Many doctors were taught the old rule and never updated their knowledge.
- Fear of lawsuits. If a patient has a reaction, the doctor might be blamed-even if the reaction was rare and the drug was appropriate.
This isn’t just academic. It’s costing lives. When doctors avoid cephalosporins because of this myth, they turn to broader-spectrum antibiotics like vancomycin, fluoroquinolones, or clindamycin. These drugs are more likely to cause C. diff infections, which can be deadly. They also drive antibiotic resistance, making future infections harder to treat.
The CDC estimates that inappropriate antibiotic choices due to mislabeled penicillin allergies cost the U.S. healthcare system over $1 billion a year. That’s billions spent on longer hospital stays, more expensive drugs, and preventable complications.
What Should You Do If You Have a Penicillin Allergy?
If you’ve been told you’re allergic to penicillin, here’s what to do next:
- Don’t assume you’re allergic for life. Most people outgrow it. Ask your doctor about allergy testing.
- Know your reaction type. Did you have hives or trouble breathing? Or just a rash or upset stomach? Write it down.
- Ask for penicillin skin testing. It’s simple, safe, and highly accurate. A negative test means you can probably take penicillin-and cephalosporins-without risk.
- If you need a cephalosporin, ask which one. Avoid first-generation unless there’s no other option. Ceftriaxone or cefepime are usually safer.
- Get your allergy status updated. If testing shows you’re not allergic, ask your doctor to remove the label from your medical record.
Even if you’ve never been tested, if your reaction was mild or happened decades ago, you’re likely safe with modern cephalosporins. The data is clear: the risk is low, the benefits are high, and the consequences of avoiding them are serious.
The Bigger Picture: Why This Matters Beyond One Drug
This isn’t just about cephalosporins. It’s about how medicine treats allergies in general. We’ve spent decades treating labels like facts. But labels are often based on old data, misunderstandings, or even miscommunication.
Penicillin allergy delabeling programs-where hospitals systematically test and reclassify patients-are now showing real results. In one study, after implementing a delabeling program, hospitals saw:
- 25% reduction in broad-spectrum antibiotic use
- 15% drop in C. diff infections
- 1-2 day shorter hospital stays
These aren’t small wins. They’re life-changing.
And it’s not just penicillin. Similar issues exist with sulfa drugs, vancomycin, and even aspirin. We need to stop treating allergy labels as permanent truths. We need to start treating them as hypotheses-something to test, not to fear.
For patients, that means asking questions. For doctors, it means updating their knowledge. For the system, it means changing labels, training, and protocols.
The next time someone says, ‘You can’t take cephalosporins because you’re allergic to penicillin,’ you now know the truth: it’s not that simple. And the right answer might just be the antibiotic you were afraid to take.
kabir das
January 28, 2026 AT 18:02Laura Arnal
January 29, 2026 AT 09:58Eli In
January 30, 2026 AT 19:53Megan Brooks
January 31, 2026 AT 00:51Ryan Pagan
February 1, 2026 AT 11:59Paul Adler
February 2, 2026 AT 05:44