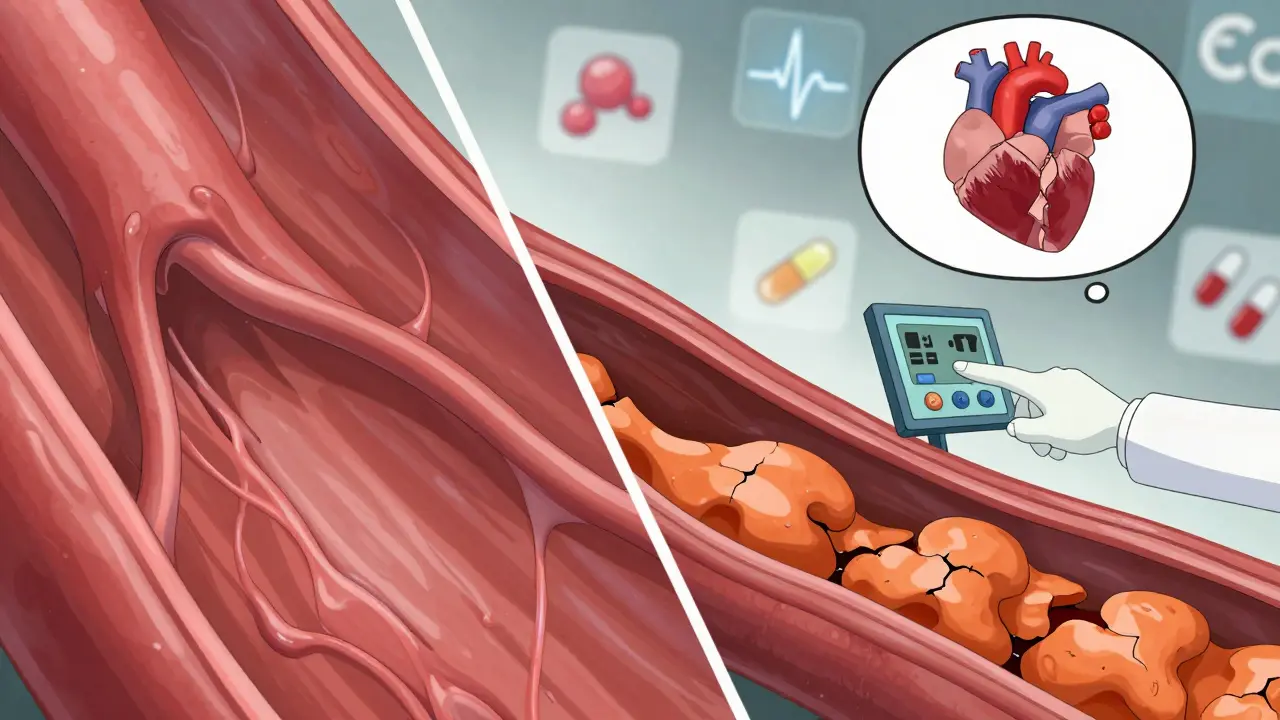
A coronary calcium score isn’t just another number on a lab report-it’s a direct look at the hidden buildup in your heart’s arteries. This simple, non-invasive CT scan detects calcium deposits that form as part of atherosclerotic plaque. And here’s the thing: you can have serious plaque buildup without feeling a single symptom. That’s why this test matters. It doesn’t wait for chest pain or a heart attack to sound the alarm. It tells you what’s happening inside your arteries right now.
What the Scan Actually Shows
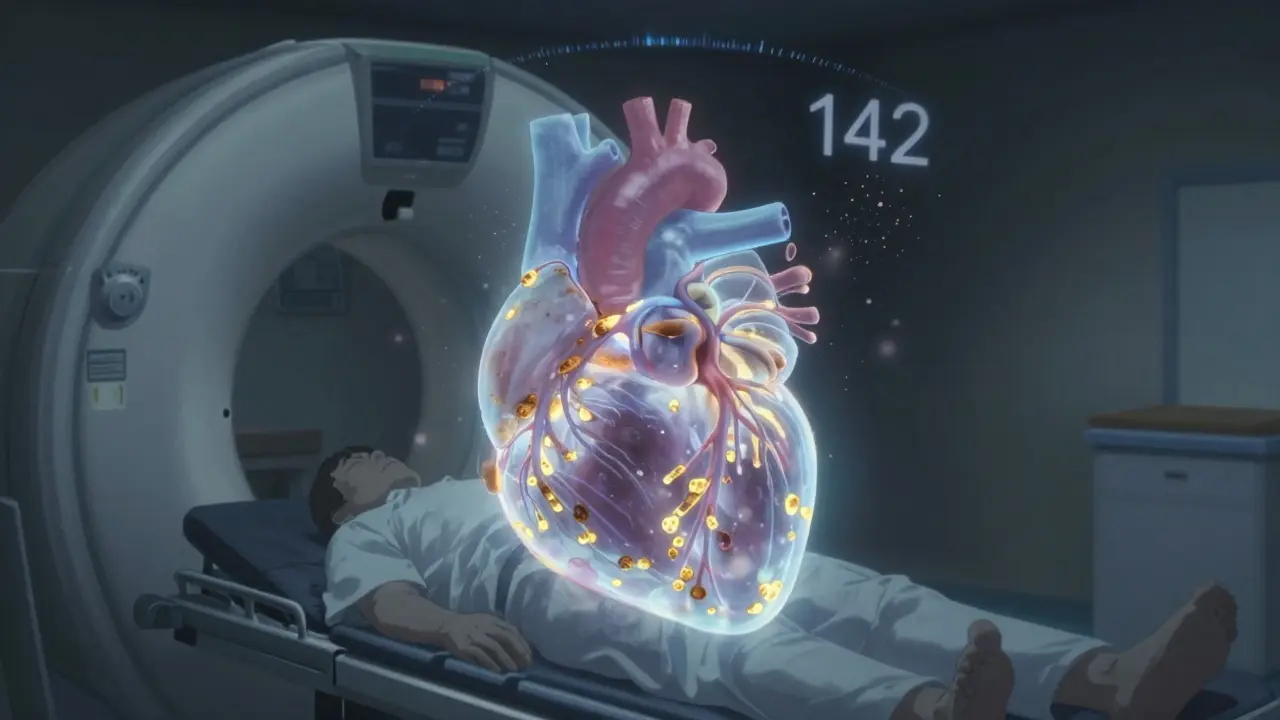
The coronary calcium scan uses a specialized CT machine to take dozens of quick images of your heart. No needles. No contrast dye. Just you lying still for about 10 seconds while the machine captures cross-sections of your coronary arteries. The computer then calculates how much calcium is present-using something called the Agatston Score, named after the radiologist who created it in 1990.
This score doesn’t measure plaque directly. It measures the calcium that gets deposited inside plaque over time. Think of it like rust on a pipe. The rust isn’t the clog itself, but it tells you there’s been a slow buildup inside. In your arteries, calcium is a sign that plaque has been forming for years. And the more calcium, the more plaque you have.
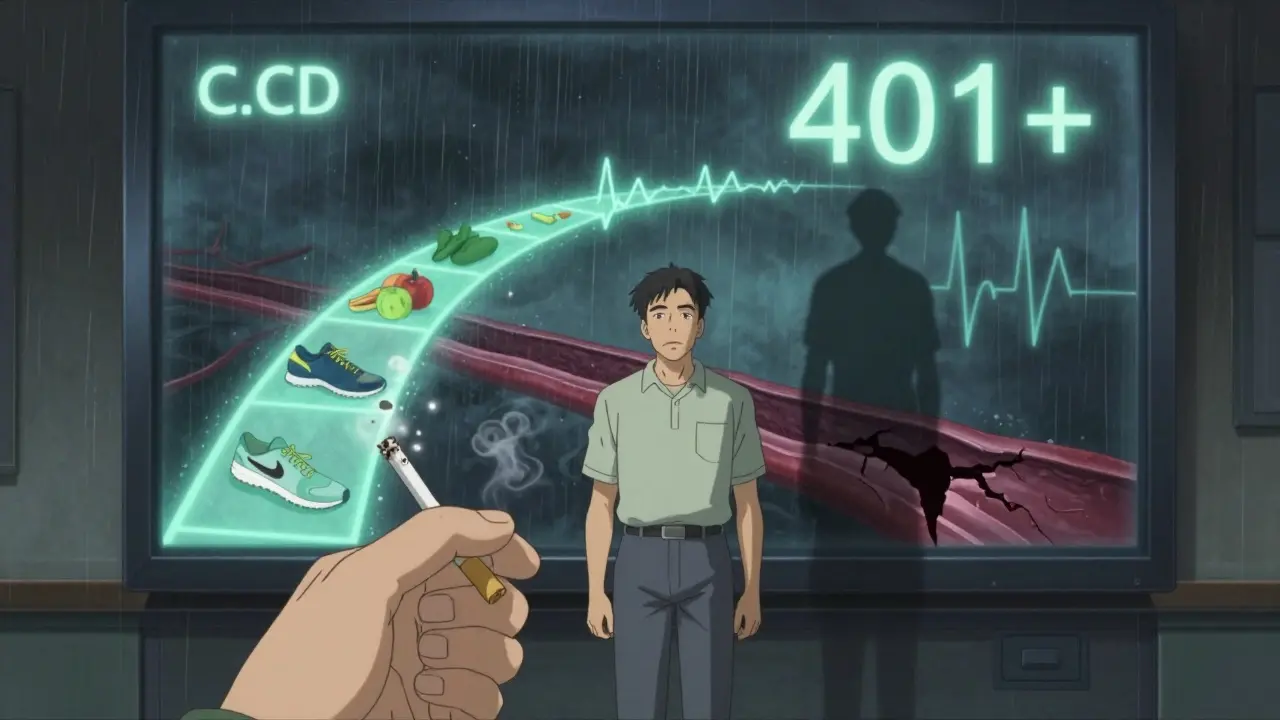
Here’s what the numbers mean, based on guidelines from the American College of Cardiology and Cleveland Clinic:
- 0 = No detectable calcium. Low risk of heart disease.
- 1-10 = Minimal plaque. Still low risk, but not zero.
- 11-100 = Mild plaque. Early signs of artery disease.
- 101-400 = Moderate plaque. Your risk of a heart event is about 75% higher than someone with a score of zero.
- 401+ = Extensive plaque. High risk. This level often means significant narrowing of arteries.
These numbers aren’t just labels-they guide real medical decisions. A score above 100, especially if you’re in your 50s or 60s, often triggers doctors to recommend statins, even if your cholesterol looks fine. Why? Because calcium is a better predictor of heart attack risk than cholesterol alone.
Why It Beats Traditional Risk Calculators
Most doctors use tools like the Pooled Cohort Equations to estimate your heart disease risk. They look at age, blood pressure, cholesterol, smoking status, and diabetes. But here’s the problem: these tools get it wrong for up to 30% of people.
Studies in Circulation show that many people labeled as “low risk” by these calculators actually have high calcium scores. They’re walking around thinking they’re fine-until they’re not. Meanwhile, others with high cholesterol and normal scores may not need aggressive treatment.
The coronary calcium score cuts through the guesswork. It doesn’t estimate risk. It measures what’s actually in your arteries. A 2021 study in the Journal of the American College of Cardiology found that adding a calcium score to traditional risk factors improved accuracy by nearly 10%. That’s huge. It means more people get the right treatment-and fewer get unnecessary medications or procedures.
What It Can’t Do
But it’s not perfect. The scan only sees calcified plaque. About 20-30% of plaque is soft and doesn’t contain calcium yet. That means a score of zero doesn’t guarantee you’re free of heart disease. It just means you don’t have hardened plaque.
That’s why a coronary calcium scan isn’t used the same way as a coronary CT angiogram (CCTA). CCTA shows both soft and hard plaque, but it requires contrast dye and delivers more radiation. It’s also more expensive. The calcium scan is the first step-cheap, fast, and low-radiation-for people who don’t have symptoms but have risk factors.
It also doesn’t work well for people with chronic kidney disease. Their arteries often calcify from mineral imbalances, not from atherosclerosis. So a high score in those patients doesn’t mean the same thing.
Who Should Get One?
The guidelines are clear: this test is for asymptomatic adults with intermediate risk-that’s a 7.5% to 20% chance of a heart event in the next 10 years. That usually means:
- Men aged 45-75
- Women aged 55-75
- With one or more risk factors: high LDL, low HDL, high blood pressure, smoking, diabetes, or family history
It’s not for people with obvious heart disease, like chest pain or a previous heart attack. It’s also not for low-risk people under 40. But if you’re in that middle zone-where your doctor says, “You’re not high risk, but you’re not low risk either”-this test can be a game-changer.
In 2023, the Society of Cardiovascular Computed Tomography updated its guidelines to include people with LDL cholesterol over 160 mg/dL-even if they have no other risk factors. That’s a big shift. It means more people are being screened based on one strong marker.
What Happens After the Scan?
Getting the score is just the start. What matters is what you do next.
If your score is zero, keep doing what you’re doing. Focus on staying active, eating well, and avoiding smoking. You’re in the best possible group.
If your score is 1-100, your doctor may suggest lifestyle changes: more exercise, less sugar, better sleep. Sometimes they’ll start you on a low-dose statin, especially if you have other risk factors.
If your score is above 100, most cardiologists will recommend a statin-usually high-intensity if it’s over 300. That’s true even if your cholesterol is normal. Why? Because the plaque is already there. The statin isn’t just lowering cholesterol-it’s stabilizing the plaque so it doesn’t rupture and cause a clot.
And here’s something surprising: many people say their score was the wake-up call they needed. One Reddit user, age 52, had a score of 142. He’d ignored his doctor’s advice to quit smoking and take statins for years. After seeing his score, he quit smoking within a week and started medication. He said, “It wasn’t the cholesterol that scared me. It was the number.”
Cost, Coverage, and Accessibility
The scan usually costs between $100 and $300 out of pocket. Many private insurers cover it if your doctor recommends it, especially if you’re in the intermediate-risk group. But Medicare doesn’t cover it yet. That’s a big barrier.
Only about 15% of eligible patients actually get tested, according to the American Heart Association. Why? Lack of awareness, insurance confusion, and some doctors still thinking it’s “experimental.” But the data is solid. The MESA study showed that adding calcium scoring to risk assessment improved prediction accuracy enough to change treatment for nearly half of intermediate-risk patients.
Some imaging centers now use AI to reduce radiation by 40% without losing image quality. That’s a recent breakthrough. The technology is getting better, faster, and safer.
What’s Next?
The National Institutes of Health is running a 10,000-patient study called the CAC Consortium Study, tracking outcomes over five years. The goal? To set exact thresholds for when to start statins based on calcium score alone.
Right now, guidelines say: if your score is over 100 and you’re 40-75, talk to your doctor about statins. If it’s over 400, you’re in high-risk territory. But soon, we may have even clearer rules.
For now, the message is simple: if you’re in that middle zone, don’t wait for symptoms. Ask your doctor about a coronary calcium score. It’s the most direct way to know if your arteries are quietly filling with plaque-and whether you need to act now to stop it.
Is a coronary calcium scan the same as a stress test?
No. A stress test checks how your heart performs under physical strain, often by monitoring your EKG while you walk on a treadmill. It can show signs of reduced blood flow, but it doesn’t show plaque buildup directly. A coronary calcium scan shows actual calcium deposits in your arteries. Stress tests have a 15-20% false positive rate. Calcium scoring gives you direct anatomical evidence, with 95% sensitivity for detecting atherosclerosis.
Can a calcium score be too high?
There’s no upper limit that’s considered “too high.” A score over 1,000 means extensive plaque and a very high risk of heart attack. But even at that level, treatment can still reduce your risk significantly. Statins, blood pressure control, and lifestyle changes can stabilize plaque and prevent rupture. The goal isn’t to lower the score-it’s to prevent complications.
Does a zero calcium score mean I’m completely safe from heart disease?
Not entirely. A zero score means no calcified plaque, which is excellent. But about 20-30% of plaque is soft and doesn’t contain calcium yet. So you could still have early, non-calcified plaque. That’s why maintaining healthy habits matters-even with a zero score. It’s the best possible outcome, but not a guarantee.
How often should I get a coronary calcium scan?
If your score is zero and you’re healthy, you might wait 5-10 years before repeating it. If your score is moderate or high, your doctor may repeat it in 2-5 years to track progression. But frequent repeat scans aren’t usually needed unless your risk factors change dramatically-like gaining a lot of weight, starting smoking, or developing diabetes.
Do I need to prepare for the scan?
Yes, but minimally. Avoid caffeine and smoking for 4 hours before the test, since they can raise your heart rate and blur the images. You don’t need to fast. Wear comfortable clothing without metal zippers or buttons near your chest. The test itself takes less than 5 minutes, and you won’t feel anything during it.
Is the radiation from the scan dangerous?
The radiation dose is low-about 1-3 mSv, similar to a mammogram or a round-trip flight from New York to Los Angeles. That’s far less than a CT scan with contrast. The benefit of detecting early heart disease far outweighs the minimal radiation risk. Newer AI-enhanced scanners can reduce this even further by 40%.
Wren Hamley
January 2, 2026 AT 04:36So let me get this straight - calcium is like rust on a pipe, and we’re using that analogy to justify throwing statins at people? Cool. I get it. But what if the ‘rust’ is just the body’s way of patching up micro-tears from chronic inflammation? Maybe we’re treating the symptom, not the cause. I’ve seen people with scores over 800 who eat whole foods, sleep 8 hours, and never touch sugar - and they’re still healthier than the 30-year-old with a score of 20 who drinks protein shakes and runs on espresso.
Calcium scoring’s useful, sure. But it’s not a crystal ball. It’s a snapshot. And we’re acting like it’s the whole damn movie.
Tru Vista
January 2, 2026 AT 06:42Zero score = safe. Right. Lol. I had a 0 and still got a MI at 48. They don’t test for soft plaque. They don’t test for endothelial dysfunction. They don’t test for your chronic stress levels. This whole thing is a money machine. Statins are big pharma’s favorite toy. Don’t believe the hype.
Hank Pannell
January 3, 2026 AT 12:55There’s a philosophical undercurrent here that’s rarely discussed: the medicalization of uncertainty. We’re not just measuring calcium - we’re measuring anxiety. The Agatston score gives us a false sense of precision in a domain that’s inherently probabilistic. A score of 142 doesn’t mean you’ll have a heart attack next year. It means you’re in a cohort with a higher probability. But probability isn’t destiny.
And yet, we treat it like a death sentence. We prescribe statins like they’re vaccines. We forget that medicine isn’t just about numbers - it’s about narratives. The man who quit smoking after his score? That’s not a biomarker victory. That’s a human one. The number was just the catalyst.
So maybe the real value of the scan isn’t in the digits - it’s in the conversation it forces. The uncomfortable one. The one where you stop blaming cholesterol and start asking why your body’s building plaque in the first place.
Lori Jackson
January 4, 2026 AT 06:37Oh please. Another ‘but what about soft plaque’ comment? Look, if you’re not willing to get a scan because you’re scared of the truth, that’s your problem. I’ve seen people with LDLs of 280 and scores of 12 - they’re fine, right? No. They’re ticking bombs. And you? You’re probably one of those people who thinks ‘natural remedies’ can dissolve arterial plaque. Go drink your turmeric lattes. I’ll be here, getting my CAC done every 3 years while you’re on your third bypass.
It’s not elitist to trust data. It’s responsible.
JUNE OHM
January 4, 2026 AT 18:59Why does Medicare not cover this?! It’s a CLEAR national security issue! Our healthcare system is being hijacked by Big Pharma and the WHO. This scan could save millions - but they don’t want you to know the truth. The government is keeping this under wraps because they profit from statins and bypasses. I’ve seen the documents. They’re hiding the real stats. You think your doctor’s telling you everything? Think again. 😡🇺🇸
Also, why is the scan only for 45+? What about Gen Z? They’re eating processed junk and vaping. We need this for EVERYONE. #CACforAll #StopTheCoverup
Ian Ring
January 5, 2026 AT 03:08Interesting piece - and I appreciate the nuance around soft plaque vs. calcified. But I’m curious: how many of these scans are being performed in primary care settings versus cardiology clinics? I’ve seen data suggesting that when GPs order these, the follow-up is often inconsistent - patients get the score, then vanish from the system.
Also, the cost barrier is real. £150 in the UK is a non-trivial sum for someone on a fixed income. I’d love to see a public health initiative - maybe bundled with annual cholesterol checks - to make this more accessible. Not everyone can afford to ‘invest’ in their arteries.
veronica guillen giles
January 5, 2026 AT 21:21Wow. Just… wow. So we’re now quantifying guilt? ‘Your calcium score is 217 - that’s basically your willpower deficit in numbers.’
Let me guess - the next thing is a ‘lung score’ for smokers, a ‘liver score’ for wine drinkers, and a ‘soul score’ for people who don’t meditate.
It’s not that I’m against prevention. It’s that I’m against turning medicine into a moral audit. You’re not a bad person because your arteries have rust. You’re a person who’s lived. Maybe the real question isn’t ‘how much calcium?’ - it’s ‘why did you stop listening to your body before it screamed?’
Palesa Makuru
January 7, 2026 AT 21:13I’m from South Africa - we don’t have access to this test unless you’re rich or have private insurance. But I’ve seen patients here with scores of 600+ and no symptoms. They’re farmers, they walk 10km a day, eat maize and beans. Meanwhile, my cousin in LA, eats kale smoothies, does yoga, and has a score of 380. What’s the real story?
Maybe the problem isn’t just plaque. Maybe it’s stress. Maybe it’s pollution. Maybe it’s sleep. We’re reducing a complex system to a single number. That’s not science - that’s simplification for convenience.
innocent massawe
January 8, 2026 AT 05:39Thanks for sharing this. I'm from Nigeria - here, most people don't even know what a CT scan is. But I showed this to my uncle who has high BP. He said, 'So if my arteries are rusting, why don't we fix the water?' 😅
It made me think - maybe in places without advanced tech, we still understand the basics: clean food, clean air, less stress. Maybe the answer isn't more scans… but less pollution.
❤️
Vincent Sunio
January 8, 2026 AT 07:52It is regrettable that the author has failed to acknowledge the methodological limitations of the Agatston scoring system - specifically, its non-linear scaling and lack of standardization across CT platforms. The claim that a score of 101–400 correlates with a 75% increased risk is misleading without adjustment for age, sex, and ethnicity. Furthermore, the cited JACC study fails to account for confounding variables such as statin adherence and dietary compliance.
While the intent is laudable, the presentation of this data as definitive clinical guidance is premature. Until prospective, randomized trials establish causality - not merely correlation - this remains a screening tool of uncertain utility. One must be cautious not to conflate association with intervention.
Angela Goree
January 8, 2026 AT 13:20Why is no one talking about the fact that calcium scoring is basically a scam? They charge you $300 to tell you what your cholesterol and blood pressure already hinted at! And then they scare you into buying statins. I’ve had 3 scans - all different numbers. Same body. Different machine. Different tech. Different radiologist. It’s not science - it’s gambling.
And don’t get me started on the AI ‘reducing radiation’ - that’s just marketing. They’re selling you peace of mind so you’ll pay for the next one in 2 years. 😒
Philip Leth
January 8, 2026 AT 14:11Man, I got my score last year - 89. I’m 51. I thought I was fine. Then I saw the number and thought: ‘I’ve been lying to myself for 15 years.’
I started walking 6 miles a day. Cut out soda. Started sleeping 7 hours. Lost 20 lbs. My doc says my LDL dropped 40 points. My BP’s normal. I didn’t need statins - I needed a wake-up call.
So yeah. This test? It’s not magic. But it’s real. And sometimes, real is all you need to finally do the right thing.
Shruti Badhwar
January 9, 2026 AT 00:53As a physician in India, I’ve seen patients with scores above 1000 who live on lentils, walk to work, and have never seen a pharmacy. Meanwhile, urban professionals with perfect scores are on 5 medications and still have angina.
This is not about calcium. It’s about epigenetics, chronic stress, and the silent toxicity of urban living. The scan is a tool - but the real diagnosis is the lifestyle we’ve chosen to normalize.
Let’s not mistake measurement for meaning.
Sarah Little
January 10, 2026 AT 20:03Can we talk about how the ‘zero score’ people are the ones who get ignored? I had a 0 at 42. My doctor said, ‘You’re golden.’ Five years later, I had a stent. The plaque was soft. No calcium. No warning. I’m now on a statin. And I’m mad. Because I was told I was fine. So if you have a zero - don’t relax. Just… don’t smoke. Ever.
Also, caffeine before the scan? I had a latte. My heart rate spiked. My score was 30 points higher than it should’ve been. So… yeah. Don’t trust the number. Trust your habits.
Hank Pannell
January 11, 2026 AT 07:13Interesting - your comment about the latte and the inflated score reminds me of something deeper. We treat these numbers like they’re immutable truths. But they’re snapshots. Taken under conditions we can’t always control. The same body, same arteries, different caffeine, different scanner, different day - and suddenly you’re ‘high risk.’
Maybe the real takeaway isn’t the number - it’s the pattern. If your score creeps up over time, even from 20 to 80, that’s the story. Not the absolute value. The trajectory matters more than the threshold.
And that’s something no algorithm can replace. Only consistent, long-term observation can reveal that.