Cumulative Drug Dose Calculator
Understand Your Medication Risk
Cumulative drug toxicity happens when medications build up in your body over time. This calculator helps you track your exposure to understand potential risks.
Key Facts About Cumulative Toxicity
- Drugs with long half-lives (over 24 hours) are most likely to accumulate
- Liver and kidney function decline with age, increasing toxicity risk
- Silent symptoms include unexplained fatigue, tremors, and memory issues
- Early detection is critical - damage can become irreversible
Your Cumulative Dose Analysis
Enter your medication details above to see your cumulative dose analysis.
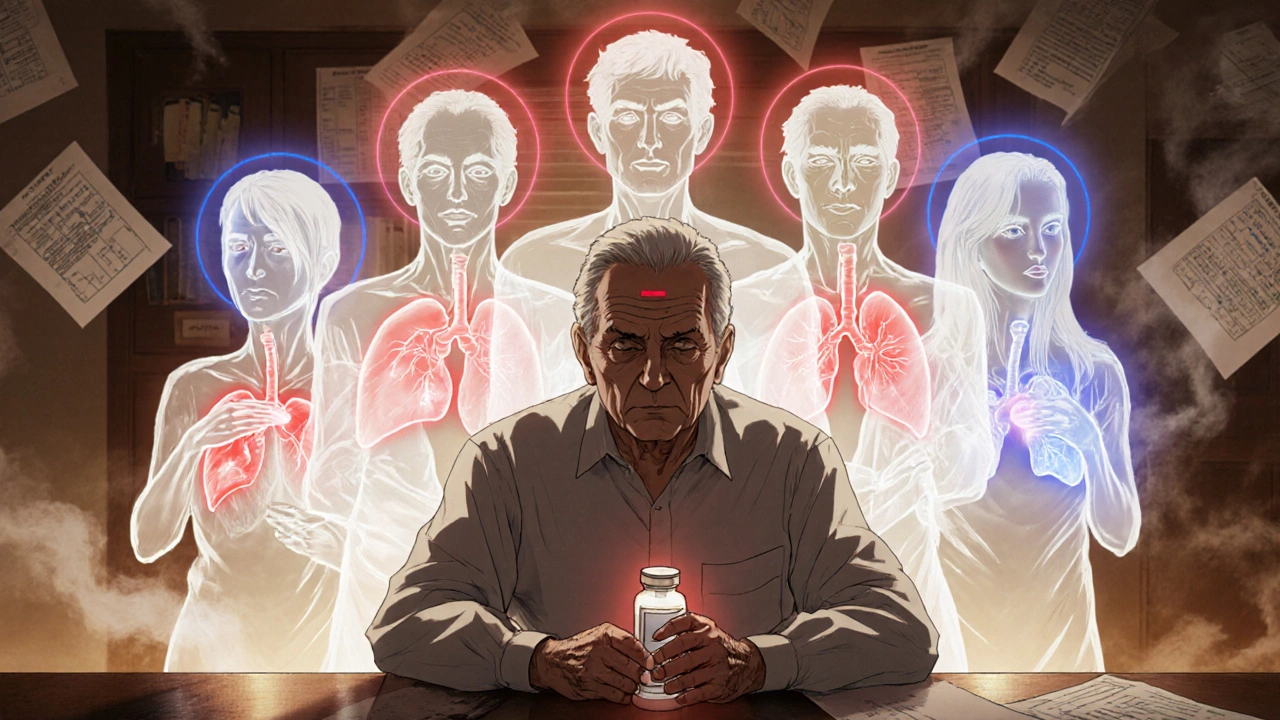
Have you ever taken a medication for months or years and suddenly started feeling worse - not because you changed your dose, but because you’ve been taking it too long? You’re not imagining it. This isn’t bad luck. It’s cumulative drug toxicity.
What Exactly Is Cumulative Drug Toxicity?
Cumulative drug toxicity happens when your body can’t clear a medicine fast enough. Instead of washing out between doses, the drug builds up like water in a sink with a slow drain. Over weeks, months, or even years, that slow leak becomes a flood. And when the concentration crosses a certain threshold, your body starts to react - not with a sudden crash, but with slow, creeping side effects. This isn’t the same as an allergic reaction or a one-time overdose. Those are acute. Cumulative toxicity is silent. It sneaks in. You might feel a little tired. Your hands might shake a bit. Your liver enzymes creep up on a blood test. You chalk it up to aging, stress, or just getting older. But it’s the drug - slowly, steadily - wearing you down. Drugs with long half-lives are the biggest culprits. If a drug takes more than 24 hours to clear half its amount from your system, it’s already on the path to building up. Think amiodarone for heart rhythm, lithium for bipolar disorder, or digoxin for heart failure. Even some antibiotics and cancer drugs do this. Fat-soluble compounds like vitamin A or D can store in your fat tissue for months. Heavy metals like lead or mercury? Those can stick around for years.Why It Hits Harder as You Age
Your liver and kidneys don’t work as well after 65. That’s not a myth - it’s science. Studies show that up to half of older adults have reduced ability to process and remove drugs. That means a dose that was safe at 45 becomes dangerous at 75. The Journal of the National Cancer Institute found that 68% of adverse drug reactions in elderly patients are due to cumulative buildup, not mistakes in dosing. Take amiodarone. It’s a lifesaver for some heart conditions. But it accumulates in the lungs. After a cumulative dose of 600 grams - yes, grams - some patients develop irreversible lung scarring. Doctors check blood levels regularly. But blood levels don’t tell the whole story. The drug is hiding in fat, in lung tissue, in the liver. By the time symptoms show, it’s often too late. The American Geriatrics Society Beers Criteria lists 34 medications with high cumulative risk for seniors. For example, anthracycline chemotherapy drugs can damage the heart. The safe lifetime limit? 450 mg per square meter of body surface. That number comes from 17 studies with over 8,500 patients. Go over it, and your heart muscle weakens. No warning. No sudden event. Just a slow decline in stamina, shortness of breath, swelling in the legs.How It Shows Up - The Silent Signs
Cumulative toxicity doesn’t announce itself with a rash or vomiting. It whispers.- Unexplained fatigue that doesn’t improve with rest
- Hand tremors you didn’t have before
- Memory lapses or brain fog
- Changes in vision or hearing
- Unusual bruising or bleeding
- Weight gain without changes in diet
- Swelling in ankles or feet
- Persistent dry cough
What Doctors Miss - And Why
Many doctors don’t track cumulative doses. Why? Because most electronic health records don’t do it automatically. You might see your oncologist every three weeks. They check your blood. They see your last dose. But they don’t add up all the doses you’ve had since 2020. The FDA Adverse Event Reporting System recorded over 12,000 cases of cumulative toxicity between 2018 and 2022. Nearly half involved blood thinners like warfarin or apixaban. Another 28% were heart medications. These aren’t rare errors. They’re systemic blind spots. Even when monitoring is done, it’s often incomplete. Therapeutic drug monitoring checks blood levels - but not tissue stores. Amiodarone can build up in the lungs without ever raising blood levels. Lithium might be fine in your blood, but slowly poisoning your kidneys. A 2022 Medscape survey found that 82% of doctors blame patient non-adherence for missed monitoring. But the real problem? The system doesn’t make it easy. No one reminds you to get a kidney function test every six months. No one tracks your total methotrexate dose since you started for rheumatoid arthritis.How to Protect Yourself
You can’t stop taking needed medication. But you can take control.- Know your drugs. Ask your pharmacist: “Is this one that builds up over time?” If they hesitate, look it up. Drugs like amiodarone, digoxin, lithium, and methotrexate are red flags.
- Track your doses. Keep a simple log: drug name, dose, start date. Use a notes app. Take a photo of your pill bottle each time you refill. It sounds old-school, but it works.
- Ask for cumulative dose checks. Especially if you’ve been on a drug for more than a year. Say: “Can we calculate how much I’ve taken total? Is it close to the safety limit?”
- Push for regular organ tests. If you’re on a drug known to affect the liver, kidneys, or heart, demand blood tests every 6-12 months. Don’t wait for symptoms.
- Don’t ignore new symptoms. If you start feeling off after years on the same pill, don’t assume it’s just aging. Bring it up. Say: “Could this be from the medication building up?”

The Bigger Picture - What’s Changing
The industry is waking up. In 2024, the European Medicines Agency made cumulative toxicity assessments mandatory for all new drugs meant for long-term use. The FDA now requires cumulative dose warnings on 78% of new cancer drugs - up from just over half in 2017. The global market for therapeutic drug monitoring is set to hit $4.7 billion by 2028. That’s because hospitals and clinics are finally realizing: you can’t just prescribe and forget. AI tools are being tested to predict individual risk. At Memorial Sloan Kettering, a model looks at 27 factors - your age, liver enzymes, genetics, other meds - to forecast your personal toxicity risk with 82% accuracy. That’s not science fiction. It’s coming to clinics soon. But until then, the burden falls on you. You’re the only one who knows how long you’ve been taking that pill. You’re the only one who notices the new tremor in your hand. You’re the only one who can ask the question: “Could this be from the drug I’ve been taking for years?”What Happens If You Do Nothing?
Left unchecked, cumulative toxicity doesn’t just cause discomfort. It causes permanent damage. - Liver fibrosis from long-term NSAIDs or antifungals - Kidney failure from repeated contrast dyes or certain antibiotics - Hearing loss from prolonged use of some diuretics - Neurological damage from lithium buildup - Heart failure from anthracyclines And once the damage is done? Often, it’s irreversible. Stopping the drug won’t fix it. The scar tissue stays. The nerves don’t recover. The heart muscle doesn’t bounce back. The cost? In the U.S. alone, cumulative toxicity leads to $1.2 billion in extra healthcare spending each year - from emergency visits to hospitalizations to long-term care.Bottom Line
Medications aren’t harmless. Even the ones you’ve taken for years. Your body changes. Your organs slow down. The drug doesn’t. And if you keep giving it to yourself - day after day, year after year - it will eventually turn on you. Don’t wait for a crisis. Don’t assume your doctor is tracking it. You are your best advocate. Know your drugs. Track your doses. Ask the hard questions. Your future self will thank you.Can cumulative drug toxicity be reversed?
Sometimes, yes - but only if caught early. Stopping the drug can stop further buildup. But if the damage is already done - like lung scarring from amiodarone or kidney damage from lithium - it often can’t be undone. Early detection through regular monitoring is the only way to avoid permanent harm.
Which medications are most likely to cause cumulative toxicity?
Common culprits include amiodarone (heart rhythm), digoxin (heart failure), lithium (bipolar disorder), methotrexate (rheumatoid arthritis), certain antibiotics like aminoglycosides, chemotherapy drugs like doxorubicin, and fat-soluble vitamins like A and D when taken in high doses over time. Even long-term use of NSAIDs or proton pump inhibitors can lead to kidney or gut damage through accumulation.
Do over-the-counter drugs cause cumulative toxicity?
Yes. Many people don’t realize that daily use of NSAIDs like ibuprofen or naproxen for years can cause kidney damage or stomach bleeding. Long-term use of antacids like omeprazole can lead to low magnesium, bone loss, or infections. Even herbal supplements like kava or comfrey can build up and harm the liver. Just because it’s sold without a prescription doesn’t mean it’s safe for long-term use.
How often should I get tested if I’m on a long-term medication?
For drugs with known cumulative risks, get blood tests every 6 to 12 months. This includes liver enzymes, kidney function (creatinine, eGFR), electrolytes, and sometimes specific drug levels (like lithium or digoxin). Your doctor should tell you what to monitor - but if they don’t, ask. Don’t wait for symptoms. Prevention beats repair.
Can I just stop taking a drug if I suspect toxicity?
Never stop a prescribed medication suddenly without talking to your doctor. Some drugs, like beta-blockers or antidepressants, can cause dangerous withdrawal. Others, like anticonvulsants, can trigger seizures. If you suspect cumulative toxicity, schedule an appointment. Bring your drug log. Ask for testing. Work with your doctor to safely adjust or switch your treatment.
Are there tools to track my cumulative drug doses?
Yes. Many pharmacies now offer apps that track your medication history. You can also use free tools like MyTherapy or Medisafe. For high-risk drugs like methotrexate or amiodarone, some clinics use custom spreadsheets or electronic alerts. If your doctor doesn’t have a system, ask if they can help you set one up. Even a simple notebook with dates and doses works.

John Power
November 28, 2025 AT 18:38Been on lithium for 12 years. Started noticing the hand tremors around year 8. Went to my doc, they said 'it's just aging.' I pushed back, asked for a level check and kidney panel. Turned out my levels were creeping up and my creatinine was elevated. We lowered the dose and added a diuretic. I'm stable now. Don't let anyone gaslight you into thinking it's 'just getting older.' Your body's telling you something.
Emily Nesbit
November 29, 2025 AT 13:01There is a critical distinction between cumulative toxicity and pharmacokinetic accumulation. The former implies irreversible tissue damage; the latter merely denotes elevated plasma concentrations. Many clinicians conflate the two, leading to inappropriate discontinuations. Always correlate clinical symptoms with objective biomarkers-serum levels alone are insufficient.
Richard Elias
November 30, 2025 AT 19:16lol so now we gotta track every pill we ever took like its some kind of cult? my grandma took digoxin for 30 years and never had a problem. stop scaring people with your spreadsheet obsession. also you spelled 'amiodarone' wrong in the post. 😂
Scott McKenzie
December 1, 2025 AT 16:23Big respect to anyone who’s been on long-term meds and stayed proactive 🙌 I’ve helped patients track their doses with free apps like Medisafe - it’s a game changer. Even just a photo of your pill bottle each month helps. You’re not being paranoid - you’re being smart. And yes, NSAIDs count too. Ibuprofen for 10 years? That’s a silent killer. 🚨
Jeremy Mattocks
December 3, 2025 AT 04:13Let me tell you about my aunt who was on methotrexate for RA for 15 years. She didn’t get tested once after year five. Started having weird bruising, then her liver enzymes went through the roof. By the time they caught it, she had early-stage fibrosis. They had to switch her to biologics and she’s been in remission since - but her liver will never fully recover. This isn’t theoretical. It’s happening to people you know. The system is broken, but your awareness? That’s your superpower. Track. Ask. Push. Don’t wait for the crash.
Paul Baker
December 3, 2025 AT 14:25my dr said my amiodarone levels were fine but my lungs were wrecked anyway 😭 i had to get a ct scan to prove it. blood tests lie. tissue doesn't. if you feel off after years on a drug its probably the drug. no cap. 🤷♂️
Zack Harmon
December 4, 2025 AT 17:43THIS IS A MASSIVE COVER-UP. BIG PHARMA DOESN'T WANT YOU TO KNOW THAT YOUR LIFELONG MEDS ARE SLOWLY KILLING YOU. THEY MAKE BILLIONS OFF THE SIDE EFFECTS. THEY SELL YOU THE NEXT DRUG TO FIX THE DAMAGE FROM THE LAST ONE. IT'S A CYCLE. THEY'RE PROFITING OFF YOUR BODY'S DESTRUCTION. I'M NOT SCARED TO SAY IT - THIS IS MEDICAL MURDER. 💀
Benedict Dy
December 6, 2025 AT 16:38The data is unequivocal: cumulative toxicity is underdiagnosed due to systemic failures in longitudinal pharmacovigilance. Electronic health records lack temporal integration of cumulative dose metrics, and therapeutic drug monitoring protocols are inconsistently applied. The burden of vigilance has been inappropriately shifted to patients without adequate education or infrastructure. Until regulatory frameworks mandate real-time cumulative dose tracking - as the EMA now requires - this remains a preventable epidemic of iatrogenic harm.
Jill Ann Hays
December 7, 2025 AT 05:11One must consider the ontological paradox: if a drug accumulates silently and no one monitors it, does it still cause harm? The answer lies not in the pharmacokinetics alone, but in the epistemological framework of medical authority. The patient's subjective experience is dismissed until it becomes objective pathology - a failure of phenomenological listening. We are not merely biochemical vessels; we are narrators of our own decline, and the system refuses to hear us until it is too late.
Jeremy S.
December 7, 2025 AT 06:21Just asked my doctor for a cumulative methotrexate total. She pulled up my chart and said, 'Oh wow, you’re at 80% of the limit.' We switched me to a biologic. Best decision ever. Seriously - just ask.