Why Electrolyte Imbalances Matter More Than You Think
When your kidneys aren’t working right, your body can’t keep potassium, phosphate, and magnesium in balance. These aren’t just numbers on a lab report-they’re the silent drivers of your heart rhythm, muscle strength, and even your breathing. A potassium level below 3.0 mEq/L can trigger a dangerous arrhythmia. A phosphate drop below 1.0 mg/dL can leave you unable to breathe on your own. And if magnesium is low, no amount of potassium replacement will fix the problem. This isn’t theoretical. In UK hospitals, over 18% of patients with advanced kidney disease develop life-threatening electrolyte shifts within 48 hours of admission. The good news? These problems are predictable, preventable, and treatable-if you know the rules.
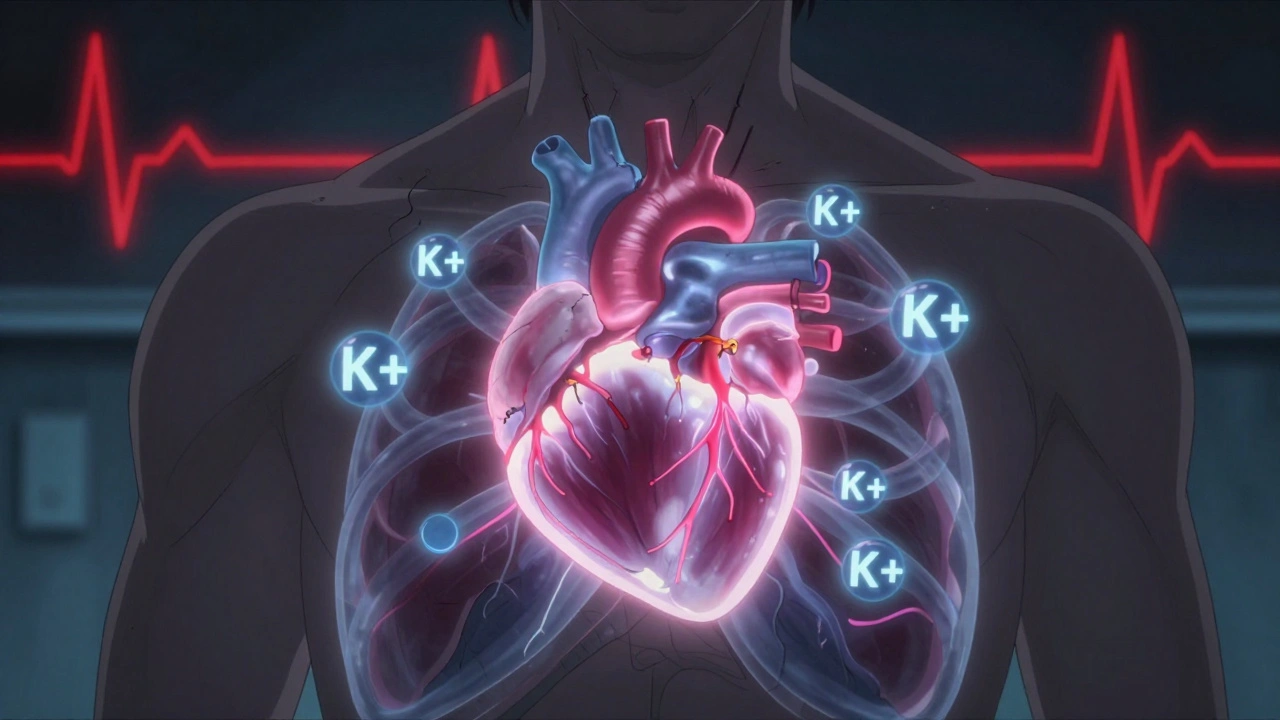
Potassium: The Heart’s Silent Guardian
Potassium keeps your heart beating regularly. Too little (hypokalemia), and your heart skips or flutters. Too much (hyperkalemia), and it can stop. Normal levels sit between 3.2 and 5.0 mEq/L. But here’s the catch: you don’t need to feel sick for potassium to be dangerously high. A level over 6.5 mEq/L with changes on an ECG is a medical emergency. That’s why every patient on dialysis, diuretics, or ACE inhibitors gets their potassium checked at least once a month.
For mild low potassium, oral supplements like potassium chloride tablets work fine. But if it’s below 3.0 mEq/L or you’re dizzy, weak, or have chest pain, you need IV potassium-slowly. The rule? Never give more than 10 mEq per hour through a peripheral IV. Faster than that, and you risk burning veins or triggering cardiac arrest. In critical cases, a central line allows up to 40 mEq/hour, but only under strict monitoring.
High potassium? Immediate action is non-negotiable. First, give calcium gluconate (10-20 mL) to protect the heart muscle. Then, insulin with glucose pushes potassium back into cells. That’s temporary. To remove it for good, you need a potassium binder like sodium zirconium cyclosilicate or patiromer-both approved by NICE in early 2023. These aren’t old-school kayexalate. They’re safer, work faster, and don’t cause bowel damage. For patients with kidney failure, dialysis is the fastest fix.
Magnesium: The Hidden Key to Potassium Recovery
Here’s what most clinicians miss: if magnesium is low, potassium won’t stay up. It’s not a coincidence. Low magnesium causes the kidneys to dump potassium like it’s trash. You give 80 mEq of IV potassium, and the level bounces back up-only to crash again in 12 hours. Why? Because magnesium was never checked.
Magnesium levels below 1.7 mg/dL are common in people on diuretics, with alcohol use disorder, or after major surgery. The normal range is 1.7 to 2.2 mg/dL. Below 1.0 mg/dL? That’s a red flag. You’re at high risk for seizures, irregular heartbeats, and muscle spasms. And yes, it worsens low calcium too.
Correction is simple: one-time IV dose of 4 grams of magnesium sulfate in 100 mL of fluid, infused over 20-30 minutes. That’s about 1 gram per minute. Don’t rush it-too fast and you’ll drop blood pressure. After giving magnesium, wait 4-6 hours before rechecking potassium. You’ll often see it rise naturally. If it doesn’t, then you know it’s not just a magnesium issue. You need to dig deeper.
Phosphate: The Forgotten Energy Source
Phosphate isn’t just for bones. It’s how your cells make energy. When levels drop below 2.5 mg/dL, you start to feel it: fatigue, confusion, muscle weakness. Below 1.0 mg/dL? That’s a crisis. Your diaphragm-the muscle you use to breathe-can fail. You’ll need ventilator support.
Why does this happen? Three big reasons: refeeding syndrome (after starvation or fasting), heavy use of phosphate binders in kidney disease, and certain IV iron treatments. In 2020, the FDA flagged ferric carboxymaltose as a major cause of phosphate crashes. If you’re getting this iron for anemia and suddenly feel weak or short of breath, check phosphate.
For mild cases, oral phosphate supplements (8 mmol per dose) work well. For severe drops, IV phosphate is needed. The standard dose is 7.5 mmol of elemental phosphorus, given slowly over 4-6 hours. Too fast, and you risk calcium dropping too hard, leading to tetany or heart rhythm problems. Always check calcium before and after. And never give phosphate to someone with kidney failure unless you’re watching them closely-too much can cause dangerous calcification in soft tissues.
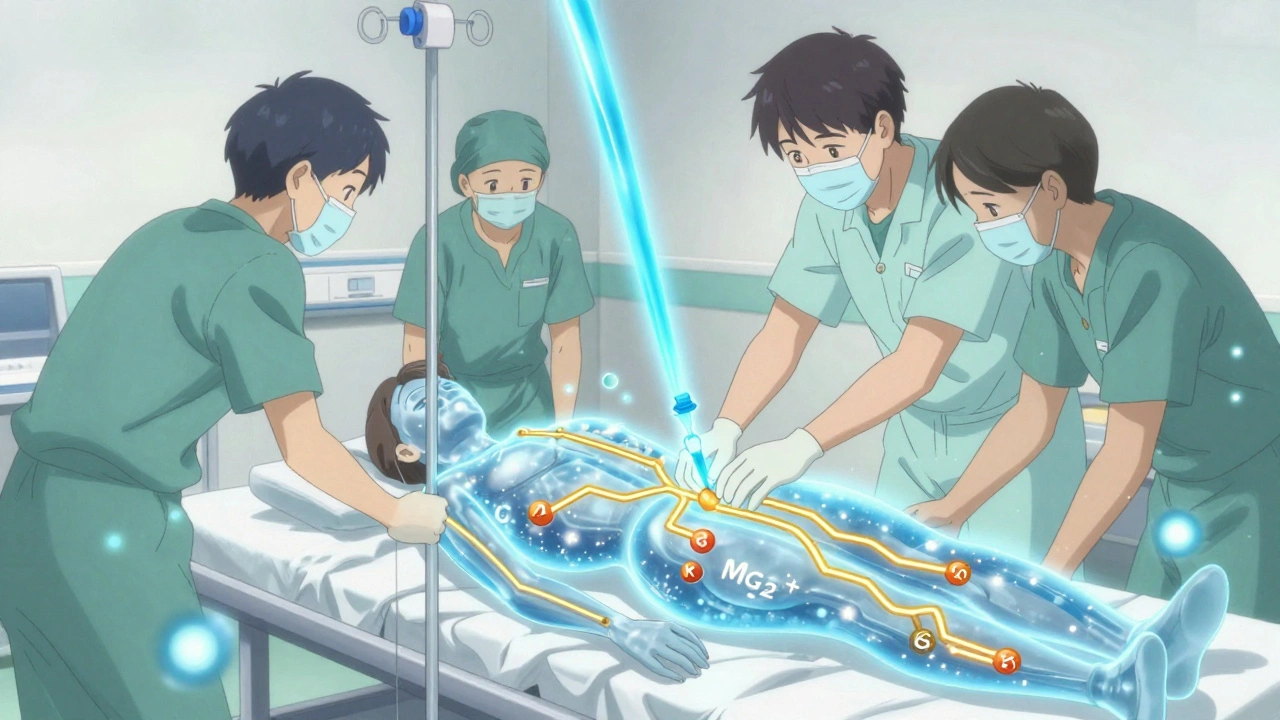
The Order of Operations: Why Sequence Matters
Managing these three electrolytes isn’t a checklist. It’s a sequence. Get it wrong, and you make things worse.
- Check magnesium first. If it’s low, replace it before touching potassium. No exceptions.
- Then fix potassium. Only after magnesium is back in range.
- Finally, assess phosphate. Especially in critically ill or malnourished patients.
This isn’t opinion. It’s in the Vanderbilt University Medical Center protocol, backed by data showing 18.7% lower mortality when followed. Many hospitals now use electronic alerts that pop up when potassium is low and magnesium hasn’t been checked in the last 24 hours. It’s not magic-it’s just smart workflow design.
Monitoring: When and How Often
Electrolytes don’t stay fixed. They shift fast. After treating high potassium, you need to check levels at 1 hour, 2 hours, 4 hours, 6 hours, and 24 hours. Why? Because insulin and glucose push potassium into cells, but the body will pull it back out. If you don’t monitor, you’ll think you’re done-then the patient crashes hours later.
For phosphate replacement, check every 6-12 hours for the first 24 hours. For magnesium, check after 4-6 hours. And always check calcium when correcting phosphate or magnesium. They’re all connected. A drop in one can drag down the others.
Point-of-care testing in emergency departments has cut the time to treatment by 37 minutes. That’s huge. In the past, patients waited hours for lab results. Now, a simple finger-prick test gives you potassium and magnesium levels in minutes. That’s saving lives.

Who’s at Risk-and What to Watch For
You don’t need to be in the hospital to get into trouble. Here are the real-world risk groups:
- People on diuretics (like furosemide): Lose potassium and magnesium daily.
- Diabetics with poor control: High blood sugar pushes potassium out of cells, then kidneys flush it.
- Chronic kidney disease patients: Lose phosphate control, retain potassium, and often take phosphate binders that make things worse.
- Those recovering from eating disorders or alcoholism: Refeeding syndrome hits hard-phosphate crashes within 24 hours of eating again.
- Patients on IV iron (ferric carboxymaltose): Watch phosphate like a hawk.
Symptoms are subtle at first: tiredness, muscle cramps, irregular heartbeat, numbness. By the time someone’s gasping for air or collapsing, it’s too late. Routine blood tests every 3-6 months for high-risk patients can catch problems before they turn deadly.
What’s New in 2025
The field has changed fast. In 2023, NICE approved two new potassium binders that are easier to take and safer than older drugs. In 2022, the FDA cleared new phosphate binders for kidney patients that don’t strip phosphate so aggressively. And in late 2024, early results from phase 3 trials showed that genetic testing can predict who’s likely to lose potassium on certain medications. Imagine a simple DNA test telling you: “You’re at high risk for low potassium on this diuretic-switch to another.” That’s coming to clinics soon.
For now, the best tool is awareness. Know your numbers. Know your risks. And never, ever skip magnesium when potassium is low.
Bottom Line
Potassium, phosphate, and magnesium aren’t separate problems. They’re a team. One falls, and the others follow. The fix isn’t just adding more of what’s low-it’s understanding the chain reaction. Check magnesium before potassium. Monitor phosphate in high-risk patients. Use new binders wisely. And never treat electrolytes in isolation. When kidneys fail, these ions become the line between life and death. Getting them right isn’t optional. It’s the foundation of safe care.
Katherine Rodgers
December 9, 2025 AT 08:22Evelyn Pastrana
December 10, 2025 AT 06:46Tejas Bubane
December 10, 2025 AT 13:47Olivia Portier
December 11, 2025 AT 17:14Tiffany Sowby
December 12, 2025 AT 02:04Jennifer Blandford
December 12, 2025 AT 04:08Brianna Black
December 14, 2025 AT 03:17Shubham Mathur
December 15, 2025 AT 22:55Stacy Tolbert
December 17, 2025 AT 06:54Ronald Ezamaru
December 18, 2025 AT 06:38Ryan Brady
December 19, 2025 AT 00:22Raja Herbal
December 19, 2025 AT 16:54Arun Kumar Raut
December 19, 2025 AT 17:47