HIT Risk Calculator
Calculate Your HIT Risk
This tool estimates your risk for Heparin-Induced Thrombocytopenia based on clinical factors. Results are for informational purposes only and do not replace professional medical advice.
Risk Assessment
Your calculated risk for Heparin-Induced Thrombocytopenia based on input factors.
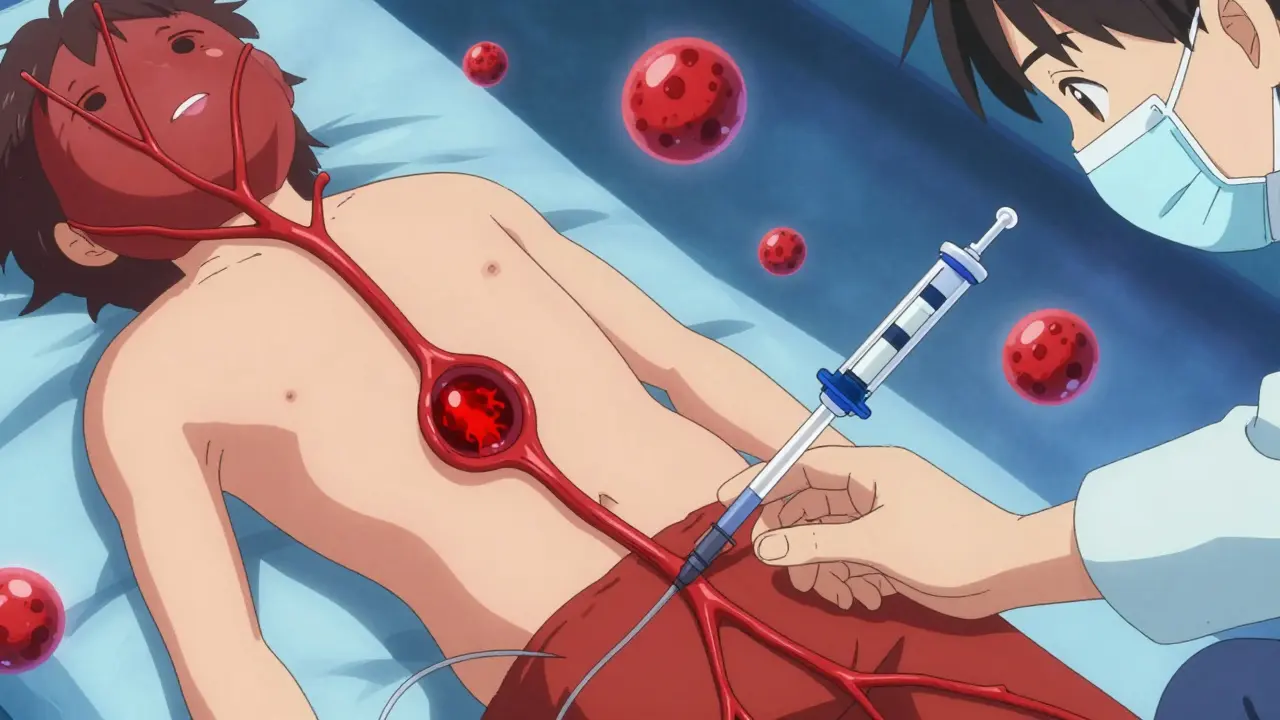
Imagine taking a blood thinner to prevent dangerous clots, only to have it cause those clots instead. That's exactly what happens with Heparin-Induced Thrombocytopenia (HIT). It's a rare but serious side effect where heparin, a common blood thinner, triggers an immune reaction that lowers platelet counts and paradoxically increases clotting risk. First documented in the 1960s despite heparin's use since the 1930s, HIT affects about 3-5% of patients on unfractionated heparin for over four days. But why does a drug meant to prevent clots cause them? Let's break it down.
What Is Heparin-Induced Thrombocytopenia (HIT)?
Heparin-Induced Thrombocytopenia (HIT)An immune-mediated reaction to heparin therapy that paradoxically causes both low platelet counts and increased blood clotting risk
HIT happens when heparin binds to Platelet Factor 4 (PF4)A protein released by platelets that forms complexes with heparin, triggering the immune response in HIT in your blood. Your immune system then creates antibodies against this complex. These antibodies activate platelets, causing them to clump together and form clots while also depleting platelet numbers. The result? A dangerous paradox: a blood thinner causing blood clots.
There are two types of HIT. Type I is harmless and non-immune, happening within 1-2 days of starting heparin. Platelets drop slightly but recover quickly without treatment. Type II is the serious immune-mediated form. It usually appears 5-14 days after starting heparin (or as fast as 1-3 days if you've had heparin recently). Type II causes significant platelet loss and high clotting risk. About 50% of Type II cases develop new or worsening blood clots, turning it into Heparin-Induced Thrombocytopenia and Thrombosis (HITT). Without treatment, HITT has a 20-30% mortality rate.
Recognizing the Symptoms: When to Suspect HIT
If you're on heparin, watch for these signs. The most common symptom is new or worsening blood clots. About 25-30% of HIT patients develop Deep Vein Thrombosis (DVT)A blood clot in a deep vein, usually in the leg, causing pain and swelling, which causes pain, swelling, warmth, and redness in the legs. Pulmonary Embolism (PE)A blood clot that travels to the lungs, causing sudden shortness of breath and chest pain happens in 15-20% of cases, leading to sudden shortness of breath, chest pain, and rapid heartbeat. Skin changes are also critical-10-15% of severe HIT cases show bruising, blackening, or blue discoloration around injection sites. Other symptoms include fever (15-20% of cases), chills (10-15%), dizziness (25%), and anxiety (20%). These symptoms often start 5-14 days after beginning heparin therapy. For example, a 65-year-old woman after knee surgery developed sudden chest pain and leg swelling on day 7 of heparin treatment, which turned out to be HIT.
Who’s at Highest Risk for HIT?
Not everyone on heparin gets HIT. Certain factors increase your risk. Women are 1.5-2 times more likely than men to develop HIT. People over 40 face 2-3 times higher risk than younger patients. Orthopedic surgery patients have the highest risk-7-10% develop HIT compared to 1-3% in medical patients and 3-5% in cardiac surgery patients. Unfractionated HeparinStandard heparin with higher risk of triggering HIT compared to low molecular weight heparin carries 2-3 times higher risk than Low Molecular Weight HeparinA type of heparin with lower HIT risk due to smaller molecular size. The longer you take heparin, the higher the risk: less than 5 days has minimal risk (<0.5%), 5-10 days raises it to 3-5%, and over 10 days increases to 5-10%. If you've had heparin in the last 100 days, re-exposure can trigger HIT within 24-72 hours due to existing antibodies.
How Doctors Diagnose HIT
Diagnosing HIT starts with the 4Ts ScoreA clinical scoring system used to assess the probability of HIT based on four criteria-a simple tool doctors use to assess risk. It scores four categories: Thrombocytopenia (platelet drop), Timing (when symptoms appear), Thrombosis (new clots), and Other causes (no other reason for low platelets). Each category gets 0-2 points. A total of 6-8 means high probability, 4-5 intermediate, and 0-3 low probability. If the score is high, doctors run tests. First, an immunoassay checks for antibodies against the heparin-PF4 complex. It's 95-98% sensitive but can give false positives. Then, a functional assay like the serotonin release assay confirms the diagnosis with 99% specificity. However, even with proper testing, there's a 1% false-negative rate. This means doctors must trust clinical judgment alongside test results.
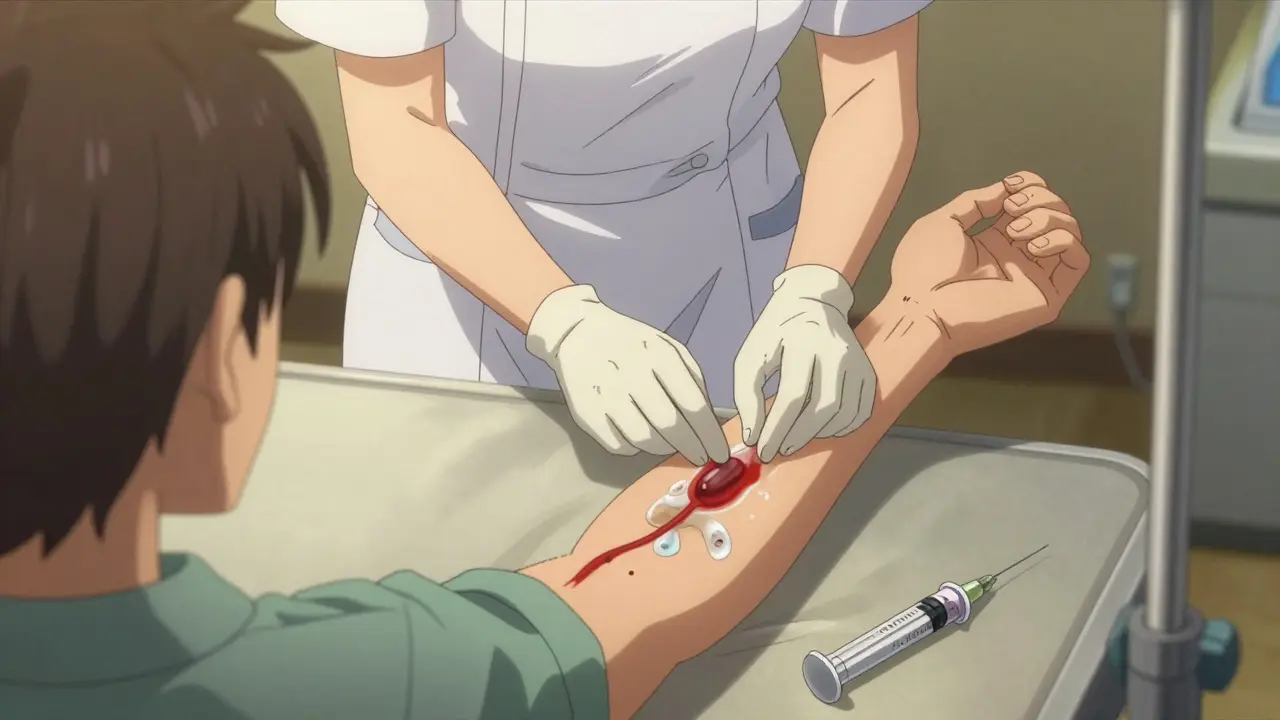
Immediate Treatment Steps for HIT
If HIT is suspected, stop all heparin immediately-including heparin flushes and heparin-coated catheters. Start an alternative anticoagulant right away. For most patients, ArgatrobanA direct thrombin inhibitor used as first-line treatment for HIT, especially in liver impairment is used at 2 μg/kg/min, adjusted to keep clotting time 1.5-3 times normal. If you have liver problems, argatroban is preferred. For cardiac surgery patients, bivalirudin is often used. FondaparinuxA factor Xa inhibitor now recommended as first-line for non-life-threatening HIT cases is now recommended as first-line for non-life-threatening cases, with 92% efficacy. Warfarin should never be started alone during HIT-it can cause skin necrosis. It can only be added after platelet counts recover above 150,000/μL and after 5 days of alternative anticoagulation. Treatment duration is 1-3 months for HIT without clots, and 3-6 months for HITT cases.
Preventing HIT: Monitoring and Safe Practices
Prevention starts with careful monitoring. Check platelet counts every 2-3 days from day 4 through day 14 of heparin therapy. If platelets drop 30% or below 150,000/μL, test for HIT immediately. Healthcare providers should know that HIT can occur with any heparin product, including low-dose flushes. In fact, 15-20% of HIT cases come from heparin-coated catheters or line flushes. Using low molecular weight heparin instead of unfractionated heparin when possible lowers risk. For high-risk patients like orthopedic surgery patients, doctors may avoid heparin altogether and use alternative anticoagulants from the start.
Is HIT the same as regular thrombocytopenia?
No. Regular thrombocytopenia from other causes like medications or infections doesn't involve the immune response triggered by heparin. HIT specifically requires heparin exposure and shows a unique pattern of platelet drop combined with increased clotting risk. The 4Ts score and specific antibody tests help distinguish HIT from other platelet issues.
Can HIT happen with low-dose heparin flushes?
Yes. About 15-20% of HIT cases are triggered by heparin-coated catheters or even small flushes. Any heparin exposure can cause HIT, though the risk is lower with smaller doses. Always inform your healthcare team if you've had heparin in the past 100 days before receiving any new heparin-based treatments.
Why can't warfarin be used alone for HIT treatment?
Warfarin alone during acute HIT can cause skin necrosis or worsening clots because it initially reduces protein C and S levels, creating a temporary pro-clotting state. It should only be added after platelet counts recover above 150,000/μL and after 5 days of alternative anticoagulation like argatroban or fondaparinux.
How long does HIT treatment last?
For HIT without thrombosis, treatment typically lasts 1-3 months. For HITT (with confirmed blood clots), treatment lasts 3-6 months. Some patients with recurrent clots or ongoing risk factors may need lifelong anticoagulation. Always follow your doctor's guidance based on your specific case.
Are there new treatments for HIT on the horizon?
Researchers are developing PF4-only immunoassays to improve diagnostic accuracy and drugs that don't interact with PF4. Two candidates are in Phase II trials, showing promise in preventing antibody formation. These could reduce HIT incidence in the future, but current treatments remain effective when used correctly.