When you pick up a bottle of pills from the pharmacy, you might think you're getting a cheap copy of your brand-name medicine. But what if that "generic" was made by the same company that made the brand? It’s not a trick-it’s called an authorized generic, and it’s a strategy used by big drugmakers to stay in control when their patents run out.
What Exactly Is an Authorized Generic?
An authorized generic is the exact same drug as the brand-name version-same active ingredient, same shape, same color, same factory, same quality control. The only difference? The label. Instead of the flashy brand name, it says the generic drug name and is sold in plain packaging. You’re getting the same pill your doctor originally prescribed, just without the marketing. This isn’t a loophole. It’s legal under the Hatch-Waxman Act of 1984, which created the modern generic drug system in the U.S. The law let companies produce cheaper versions of expired patents-but it also let the original makers play along. Pfizer, Johnson & Johnson, and other big names use this to keep some of the market share when competitors rush in with their own generics.Why Do Brand Companies Make Their Own Generics?
Patents last 20 years, but most drugs only have 7-12 years of real market exclusivity after FDA approval. Once that ends, generic makers flood the market. Prices drop fast-often by 80% in the first year. If you’re a brand company, that’s a huge hit. Instead of watching your revenue vanish, you launch your own generic. You keep control of production. You keep your factory running. You keep your supply chain intact. And you capture 15-35% of the generic market right away, according to Drug Patent Watch’s 2023 data. Take Eli Lilly’s Cialis. When the patent expired in 2018, they rolled out their own authorized generic. Even with competition, they kept 78% of the total revenue. That’s because many patients and doctors didn’t switch-they just kept taking the same pill, now labeled differently.How Is It Made? Same Factory, Same Process
You don’t need a new plant. You don’t need new equipment. You don’t need to reprove the drug works. The brand manufacturer already has FDA approval for the drug. All they do is file a simpler application called an ANDA (Abbreviated New Drug Application) and change the label. The production line stays exactly the same. The same workers, the same machines, the same quality checks. That’s why authorized generics often score higher in patient satisfaction than traditional generics. On Drugs.com, authorized generics average 4.2 out of 5 stars. Traditional generics? 3.8. The transition takes 6-9 months for regulatory paperwork and labeling changes. Compare that to traditional generics, which can take 17 months just to get FDA approval. That’s why brand companies can launch their authorized version on day one of patent expiry-like Teva did with Copaxone in 2019. They captured 22% of the market in the first quarter.
It’s Not Always Cheaper-Here’s Why
Here’s the catch: authorized generics aren’t always the cheapest option. They’re usually priced 10-15% below the brand name, but 5-10% above the competition. So if your brand drug costs $120, the authorized generic might be $105, while another generic is $80. Why? Because the brand company still needs to cover costs and make a profit. They’re not giving it away. And they know many patients won’t switch if the pill looks and feels familiar. A 2023 Reddit thread with 147 comments showed mixed reactions. One user wrote: "I paid $85 for the "generic" from my brand maker. My local pharmacy had the same pill for $30. I felt tricked." That’s not uncommon. Independent pharmacists surveyed by the National Community Pharmacists Association in 2022 said 63% of patients were confused-thinking they were getting a cheaper alternative when they weren’t.Regulators Are Watching
The Federal Trade Commission (FTC) doesn’t love this strategy. They’ve filed lawsuits against companies they believe are using authorized generics to block real competition. In 2017, Actavis settled for $448 million after the FTC accused them of using an authorized generic to delay cheaper competitors from entering the market for Namenda. The law allows authorized generics-but not if they’re used as a tool to shut out other manufacturers. The CREATES Act of 2019 tried to close some of those loopholes by making it harder for brand companies to refuse to supply samples to generic makers. Still, the practice is growing. Between 2020 and 2023, the top five drug companies introduced 47 authorized generics. That’s a 28% jump year over year.What Patients Really Think
A 2023 Kaiser Family Foundation survey of 2,000 patients found 71% preferred authorized generics-when they knew what they were. But 64% didn’t realize the company making the "generic" was the same one that made the brand. Patients like them because they’re familiar. "It’s the same pill I’ve been taking for 10 years," one review said. No surprises. No new side effects. No wondering if the generic works the same. But the lack of transparency is a problem. If you’re paying $105 for an authorized generic and a true generic is $70, you’re paying more than you need to. And if you’re on a fixed income, that $35 difference adds up.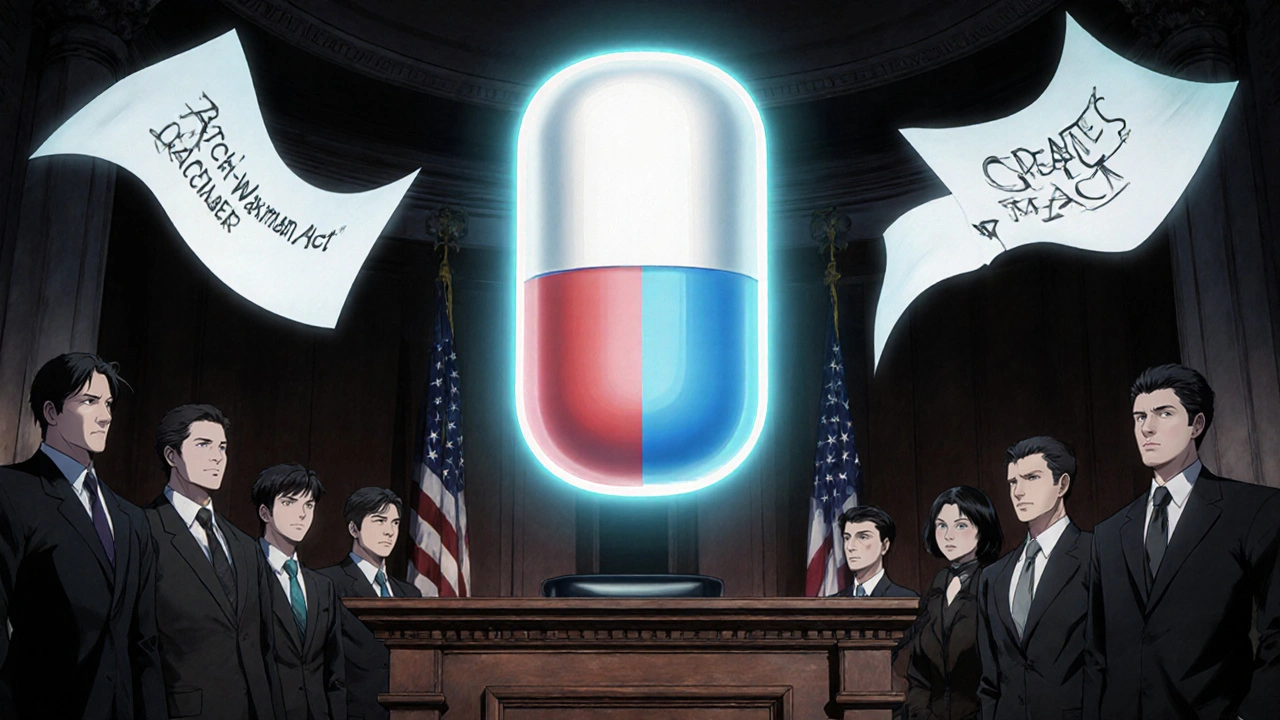
The Future: Biologics and Beyond
This strategy is moving into new territory. The first authorized biosimilar-Amgen’s version of its own Enbrel-was approved in 2023. Biosimilars are complex drugs made from living cells, not chemicals. Making them is expensive and hard. Only a few companies can do it. That means when patents expire on these drugs, there won’t be dozens of competitors rushing in. Instead, the original maker might be the only one who can produce a version. Authorized biosimilars could become the norm, not the exception. Companies like Novartis are already planning ahead. With their heart failure drug Entresto, they started positioning it for a transition to an authorized generic before the patent even expired. It’s not just about reacting to patent cliffs anymore-it’s about designing the product lifecycle from day one.What You Should Know as a Patient
If you’re on a brand-name drug that’s about to go generic, ask your pharmacist: "Is there an authorized generic?" If there is, compare the price. It might be worth it for the familiarity-but it might not be the cheapest. Don’t assume "generic" means "cheapest." Sometimes, the real generic from a different company is far cheaper. Always check the label. If it says the same company name as your brand, you’re getting an authorized version. And if you’re confused? Ask. Pharmacists can tell you exactly what you’re getting. You deserve to know if you’re paying more for the same pill.Are authorized generics the same as regular generics?
Yes and no. Authorized generics are made by the same company that makes the brand-name drug, using the same ingredients, equipment, and factory. Regular generics are made by other companies, often with different fillers or manufacturing processes. Both are FDA-approved and bioequivalent, but authorized generics are physically identical to the brand.
Why are authorized generics sometimes more expensive than other generics?
Because the brand manufacturer doesn’t want to give away their profits. They price authorized generics just below the brand name to keep some revenue, but above competing generics to avoid cannibalizing too much. It’s a strategic price point-not a discount.
Can I ask my doctor to prescribe an authorized generic?
Yes. Doctors can write prescriptions for the generic name, and pharmacies can fill it with any approved version-including the authorized one. If you prefer the authorized version, ask your pharmacist to check availability and pricing.
Do authorized generics have the same side effects as the brand?
Yes. Since they’re made with the exact same ingredients and process, side effects are identical. Many patients report fewer issues with authorized generics because they’ve already tolerated the brand version.
Is the authorized generic program good for consumers?
It’s complicated. Authorized generics provide a familiar, high-quality option and increase overall competition, which helps lower prices. But they can also delay true generic competition and confuse patients into paying more than necessary. The benefit depends on whether you value consistency over cost.

Esperanza Decor
November 10, 2025 AT 19:50So let me get this straight-pharmacies are selling the exact same pill under a different label, and patients think they’re saving money when they’re not? That’s not just misleading, it’s systemic. I’ve been on the same medication for years, and I had no idea my "generic" was made by the same company. I feel like I’ve been played.
Deepa Lakshminarasimhan
November 11, 2025 AT 16:29Big Pharma’s got a whole playbook. First they raise prices for 10 years, then they make a "generic" that’s almost the same but costs 20% more than the real one. They even own the factories. Who’s really controlling the market? Not the FDA. Not the pharmacies. It’s all just a money machine with a legal coat of paint.
Erica Cruz
November 13, 2025 AT 03:03Let’s be real-this isn’t innovation, it’s corporate theater. They’re not trying to help patients; they’re trying to keep their profit margins intact. And the fact that patients *prefer* the authorized version? That’s not because it’s better-it’s because they’ve been conditioned to trust the brand. Marketing wins again. 4.2 stars? Please. That’s brand loyalty, not clinical superiority.
Johnson Abraham
November 14, 2025 AT 20:31so like… if i get the "generic" from the same company as the brand, am i just paying extra for the same thing? lol. why do they even bother? also, why does my pharmacy not tell me this? 🤡
Shante Ajadeen
November 15, 2025 AT 03:31Good info here. I didn’t know this was a thing. If you’re on a tight budget, always check the price of the independent generic-it’s often way cheaper. But if you’ve had side effects before or just want peace of mind, the authorized one might be worth it. Just know what you’re paying for.
dace yates
November 15, 2025 AT 09:57Wait, so if the authorized generic is made in the same factory with the same process, why do some patients report fewer side effects with it than with other generics? Is it placebo? Or are the inactive ingredients actually different even if the active ones are the same?
Danae Miley
November 16, 2025 AT 23:58The FTC has repeatedly flagged this practice as anti-competitive, yet it continues to grow. This isn’t just a gray area-it’s a deliberate exploitation of regulatory loopholes. The Hatch-Waxman Act was meant to increase access, not enable monopolistic behavior under the guise of competition. The data shows a clear correlation between authorized generic launches and delayed entry of true generics. That’s not market efficiency; that’s market manipulation.
Charles Lewis
November 17, 2025 AT 02:16It’s important to contextualize this within the broader pharmaceutical ecosystem. The development of a single new drug can cost upwards of $2.6 billion, and the patent system exists to incentivize that risk. When patents expire, companies aren’t just trying to maximize profit-they’re trying to recoup investment and fund future innovation. Authorized generics represent a pragmatic middle ground: they maintain supply chain stability, preserve jobs, and ensure consistent quality while still introducing price competition. The real issue isn’t the existence of authorized generics-it’s the lack of patient education and transparency in pricing. If pharmacies and prescribers made the distinction clearer, patients could make informed choices. Instead, we’ve created a system where confusion is the default.
Renee Ruth
November 17, 2025 AT 18:27They’re not just making generics-they’re making patients feel guilty for wanting cheaper options. "Oh, you want the real generic? That’s not as good." No, it’s just cheaper. And if you’re paying $105 for the same pill that someone else gets for $30, you’re not being loyal-you’re being exploited. This isn’t about quality. It’s about control. And it’s disgusting.