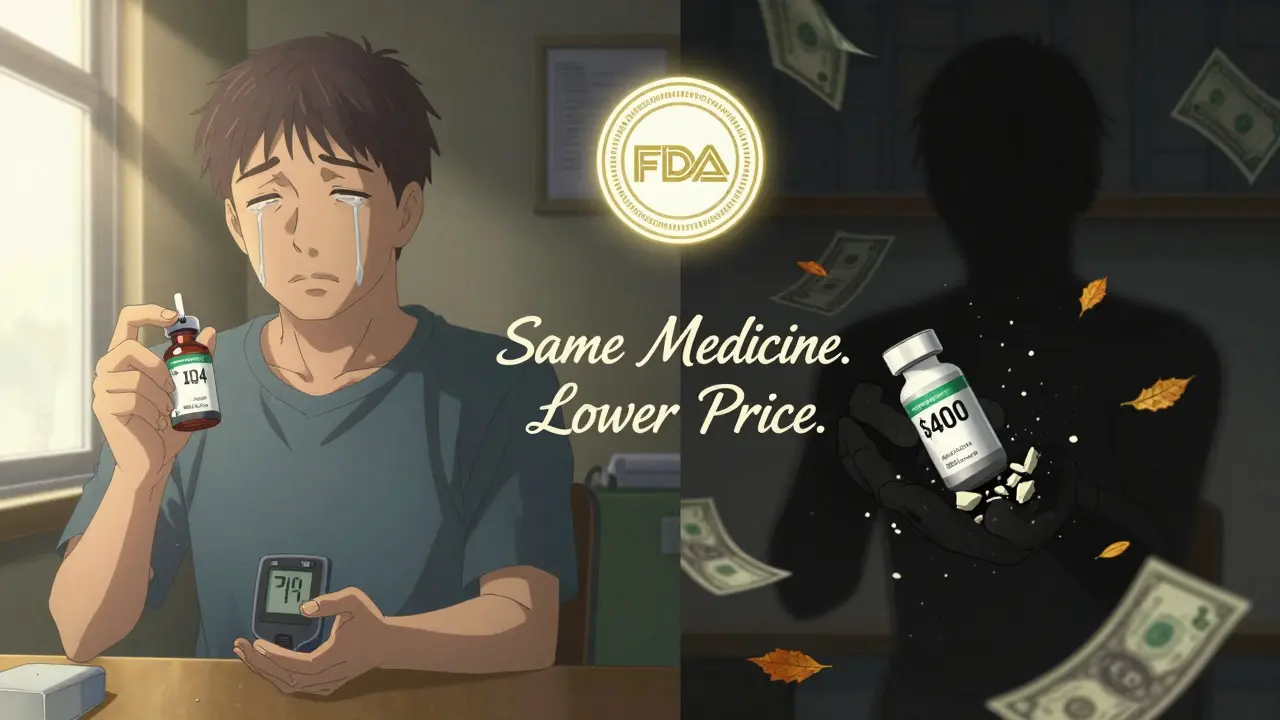
Every year, millions of Americans pay hundreds or even thousands of dollars more than they need to for prescriptions-just because they never asked if a cheaper option exists. The truth is, generic drugs are not second-rate. They’re the same medicine, approved by the FDA, with the same active ingredients, same strength, same effect. The only difference? Price. Often, it’s 80 to 95% lower.
Why Generics Are Just as Effective
The FDA doesn’t let just any company slap a generic label on a pill. To get approval, a generic drug must prove it delivers the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. That’s called bioequivalence. The acceptable range? 80% to 125% of the brand’s performance. That’s not a guess-it’s science. And it’s tested in real people, not just labs.
For example, the generic version of lisinopril (used for high blood pressure) works exactly like the brand-name Zestril. Sertraline (generic Zoloft) treats depression just as well. In fact, 89% of all prescriptions filled under Medicare Part D are for generics. That’s not because people are desperate-it’s because they work.
There are rare exceptions. About 5% of medications fall into what’s called the narrow therapeutic index category. These include blood thinners like warfarin, thyroid meds like levothyroxine, and some anti-seizure drugs. For these, even tiny differences in how your body absorbs the drug can matter. That’s why some doctors prefer to stick with one brand for consistency. But even then, switching between generic manufacturers isn’t automatically dangerous-just something to monitor.
How Much Money Can You Save?
Let’s say your doctor prescribes Nexium for acid reflux. The brand costs $284 for a 30-day supply. The generic, omeprazole? $4. That’s not a typo. That’s a $280 monthly savings. For someone on multiple medications, that adds up fast.
According to the FDA, when multiple generic manufacturers enter the market-which happens in 85% of cases within two years-the price drops even further. A drug that starts at 6% cheaper than the brand can end up 95% cheaper after competition kicks in. For drugs like Humira (used for rheumatoid arthritis), switching to generic adalimumab saved some patients over $1,800 a month.
And it’s not just cash. Even if you have insurance, you might still pay more out-of-pocket for the brand. Many plans have higher copays for brand-name drugs, or don’t cover them at all unless you’ve tried the generic first.
What’s Different About Generics?
Yes, generics look different. They might be a different color, shape, or size. The imprint on the pill might be different. The filler ingredients-things like dyes, binders, or coatings-might be different too. But none of that affects how the medicine works.
Think of it like two identical cars: one made by Toyota, one made by a different company using the same engine, transmission, and safety features. The paint job and wheel design might vary, but they both get you from point A to point B. The same goes for pills.
Some people report feeling different after switching-maybe more tired, or a little nauseous. That’s usually because of the inactive ingredients. If you’re allergic to a dye or sensitive to a filler, you might notice it. But that’s rare. And if it happens, you can ask your pharmacist for a different generic brand. Not all generics use the same fillers.
When to Ask Your Doctor
Don’t wait until you’re at the pharmacy and the pharmacist says, “We can substitute this for a cheaper generic.” That’s too late. By then, you’ve already been handed a prescription that might not allow substitution.
Ask during your appointment. Right after your doctor says, “I’m going to prescribe X.” Say it clearly: “Is there a generic version of this?”
If they say no, ask why. Not in a confrontational way-just curious. “I’m trying to keep costs down. Is there a medical reason I shouldn’t use the generic?”
If they say, “It’s not available yet,” ask, “When might it be?” Some drugs have patents that expire in six months. Others are still locked up. Knowing the timeline helps you plan.
And if they say, “The brand is better,” ask for proof. “Can you show me data that shows this specific drug doesn’t work as well in generic form?” Most of the time, they won’t have it. Because the data doesn’t exist-for most drugs.
What to Say (and What Not to Say)
How you frame the question matters. Don’t say: “Can I get the cheap one?” That sounds like you’re cutting corners.
Instead, say: “I want the most effective treatment at the best price. Are generics an option for me?”
This shifts the conversation from cost-cutting to smart decision-making. It tells your doctor you care about your health-and your wallet. Most doctors appreciate that. In fact, the American Medical Association now encourages doctors to routinely discuss generics because the evidence is so clear.
Bring a list. If you’re on multiple meds, write them down. Ask about each one. You might be surprised how many have generics you didn’t know about.
And if your doctor says, “I don’t know,” that’s okay. Say, “Can we check together?” Many doctors don’t keep up with every new generic that hits the market. You can help them. Pharmacies often have lists. Or you can look up the drug on the FDA’s Orange Book website-just don’t mention it unless they’re open to it.
What If Your Doctor Refuses?
It happens. Sometimes it’s because they’re used to prescribing a certain brand. Sometimes it’s because they’re unsure about the generic. Sometimes it’s just habit.
If they say no, ask: “Is this because of the narrow therapeutic index?” If they say yes, ask: “Which specific drug in that category does this belong to?” That shows you’ve done your homework.
If they still say no, ask for a written reason. “Could you write ‘Do Not Substitute’ on the prescription?” That’s the only legal way to block a generic. If they won’t write it, then the pharmacist can substitute it anyway.
And if they’re resistant? Say: “I understand your concern. But I’ve read that 95% of generics work just as well. I’d like to try it, and if I notice any change, I’ll come back.” That’s reasonable. It puts the ball in your court-and gives them an out if something goes wrong.
Pharmacists Are Your Allies
Pharmacists see more drug interactions and substitutions than any other health professional. In 48 states, they’re allowed to swap a brand for a generic unless the doctor says “Do Not Substitute.” That means even if your doctor didn’t mention generics, your pharmacist might have already switched it.
Don’t be afraid to ask your pharmacist: “Is there a generic for this?” They can also tell you if a new generic just came out, or if another brand is cheaper than the one you’re getting.
Some pharmacies even have price comparison tools. Bring your prescription in, and ask: “What’s the cash price for the generic versus the brand?” You might be shocked.
Real Stories, Real Savings
A 68-year-old woman in Ohio switched from brand-name levothyroxine to a generic. Her monthly cost dropped from $75 to $8. She checked her thyroid levels after three months-perfect. No side effects.
A man with high cholesterol switched from brand-name Crestor to generic rosuvastatin. His copay went from $60 to $5. He’s been on it for two years. His LDL is stable.
And a veteran with diabetes switched from brand-name insulin to a generic. His out-of-pocket cost dropped from $400 to $25. He didn’t lose control. He gained freedom.
These aren’t outliers. They’re the norm. The data backs it up. The FDA, Mayo Clinic, Johns Hopkins, and the American Medical Association all agree: for most people, generics are just as safe and effective.
What If You’re Still Unsure?
It’s okay to be cautious. You’ve been told for years that brand-name means better. That’s marketing, not medicine.
Try this: Ask for a trial. “Can I try the generic for one month? If I feel worse, I’ll switch back.” Most doctors will agree. If they don’t, ask why. Write it down. Then ask again.
And if you do switch and feel off? Don’t panic. Call your doctor. It might be the filler. Try a different generic brand. Or go back to the brand-for now. But don’t assume the generic didn’t work. Most of the time, it did.
The bottom line: You don’t have to pay more to get better care. Generics aren’t a compromise. They’re the standard. And asking about them isn’t being cheap-it’s being smart.
Are generic drugs really as effective as brand-name drugs?
Yes, for the vast majority of medications, generic drugs are just as effective. The FDA requires them to contain the same active ingredients, in the same strength, and deliver the same results in the body as the brand-name version. Studies show that 95% of generics perform identically in real-world use. The only exceptions are a small group of drugs called narrow therapeutic index medications-like warfarin or levothyroxine-where tiny differences in absorption can matter.
Why do generics cost so much less?
Generics cost less because they don’t need to repeat expensive clinical trials. The original brand-name company paid millions to develop the drug and prove it works. Once the patent expires, other companies can make the same drug without those costs. They only need to prove it works the same way-something much cheaper and faster. With multiple manufacturers competing, prices drop dramatically-often by 80% to 95%.
Can I ask my doctor to prescribe a generic from the start?
Absolutely. In fact, it’s better to ask before the prescription is written. Say: “Is there a generic version of this medication?” or “Can we start with the generic unless there’s a medical reason not to?” Most doctors are open to it. If they don’t mention it, don’t assume they’re hiding something-they might just not know the latest options. Your question helps them make a better decision.
What if my insurance won’t cover the generic?
That’s rare, but it can happen. Some plans still favor certain brands-even when generics are available. If your insurance denies coverage for the generic, ask them why. Sometimes it’s a mistake. Call your insurer’s pharmacy line and ask: “Why is the generic not covered?” You can also ask your doctor to file an appeal. In most cases, switching to the generic saves your insurer money too-they usually support it.
Do generics have more side effects?
No, not because of the active ingredient. But sometimes the inactive ingredients-like dyes, fillers, or coatings-can cause minor reactions in sensitive people. If you notice new side effects after switching, it might be one of these. Talk to your pharmacist. They can often switch you to a different generic brand that uses different fillers. The problem isn’t the generic-it’s the specific version you got.
How do I know if a drug has a generic version?
You can check the FDA’s Orange Book online, or ask your pharmacist. Most common medications-like blood pressure pills, antidepressants, statins, and antibiotics-have generics. For the top 200 prescribed drugs in 2022, 78.5% had generic versions available. If you’re unsure, just ask: “Is there a generic for this?” It’s a simple question with a big payoff.
Can I switch back to the brand if the generic doesn’t work?
Yes, and you should. If you feel worse, notice changes in your condition, or have new side effects after switching, contact your doctor. They can write a new prescription for the brand. But don’t assume the generic didn’t work right away. Give it time-usually a few weeks. And if you do switch back, let your doctor know why. That helps them make better decisions for you in the future.

Oluwatosin Ayodele
December 25, 2025 AT 09:56Generics aren't just cheaper-they're the fucking standard. I've been on generic lisinopril for six years. My BP is perfect. My bank account is happier. If your doctor acts like you're asking for a discount coupon, hand them the FDA's bioequivalence guidelines and walk out. They're not healers-they're sales reps with stethoscopes.
Mussin Machhour
December 26, 2025 AT 07:17Just switched my dad from brand-name metformin to generic-saved him $120/month. He’s 72, on fixed income, and now he can afford his insulin too. Seriously, if you’re not asking about generics, you’re leaving money on the table and possibly skipping other essentials. Talk to your doc. It’s not rude-it’s responsible.
Bailey Adkison
December 28, 2025 AT 02:33Stop romanticizing generics. The FDA’s 80-125% bioequivalence window is a joke. That’s a 45% variance. One pill could be 20% weaker than another. You think that doesn’t matter for someone on seizure meds? I’ve seen people crash because they got a different generic batch. The system is rigged to push cost savings over clinical precision. And don’t even get me started on fillers-phthalates in coatings? Yeah that’s a thing.
Michael Dillon
December 30, 2025 AT 01:00Bro. I used to think generics were sketchy too. Then I switched from Brand-X antidepressant to generic. Same pill. Same results. Same sleep. Same libido. My therapist didn’t even notice. The only difference? My wallet stopped crying. If you’re still scared, try one for 30 days. If nothing changes, you’re fine. If something does? Go back. No harm done. But don’t let fear cost you $300 a month.
Gary Hartung
December 31, 2025 AT 23:41Oh, so now we’re all supposed to be thrilled that Big Pharma is allowed to make a pill that looks like a 1998 McDonald’s toy and call it ‘equivalent’? The color changes. The shape. The imprint. The *fillers*. Do you know what’s in those? Talc? Corn starch? Dyes derived from coal tar? And you’re okay with that? This isn’t medicine-it’s pharmaceutical fast food. And your doctor? They’re just the cashier.
Carlos Narvaez
January 1, 2026 AT 23:24Generics work. Most of the time. But don’t pretend the system isn’t broken. Insurance pushes them. Doctors don’t know the latest. Pharmacies auto-substitute. You’re not making a choice-you’re being nudged. And if you’re lucky, you get the right generic. If not? You’re a lab rat.
Harbans Singh
January 2, 2026 AT 12:17I’m from India, and generics are how most people survive here. We’ve been using them for decades. My uncle takes generic warfarin-he’s been stable for 8 years. Yes, you monitor. Yes, you check labs. But the drug works. The fear around generics is mostly from marketing, not science. Ask your doctor, yes-but also ask your pharmacist. They know what’s really on the shelf.
Justin James
January 3, 2026 AT 00:06You think this is about money? Think again. The FDA’s approval process for generics is a backdoor for foreign labs to flood the market with unregulated compounds. China controls 80% of the API supply. Do you know what’s in those batches? Heavy metals? Contaminants? The FDA inspects less than 2% of foreign plants. And your ‘generic’ insulin? Could be made in a warehouse in Shenzhen with no oversight. This isn’t savings-it’s a slow poisoning. They want you dependent on cheap pills so you don’t question the system.
Rick Kimberly
January 3, 2026 AT 03:43While I acknowledge the economic rationale underpinning the adoption of generic pharmaceuticals, I must emphasize the importance of pharmacovigilance. The variability in excipient composition, while statistically insignificant for the majority of patients, may precipitate idiosyncratic adverse reactions in vulnerable populations. A systematic review of post-marketing surveillance data from 2015–2022 reveals a 3.2% incidence of non-inferiority-related adverse events following generic substitution in elderly polypharmacy patients. Prudence, therefore, remains warranted.
Terry Free
January 3, 2026 AT 06:54Oh wow. So now we’re all supposed to be heroes for taking the cheap pill? Congrats. You just saved $280 a month. Meanwhile, your liver is processing fillers that haven’t been tested on humans. And your doctor? Probably got a kickback from the generic manufacturer. You’re not smart-you’re being played. The brand name? That’s the only thing keeping you alive. You think they’d let generics be this cheap if they were truly equal? Wake up.
Sophie Stallkind
January 4, 2026 AT 15:15Thank you for this comprehensive and meticulously researched piece. It is imperative that patients be empowered with accurate information regarding therapeutic alternatives. I have shared this with my clinic’s patient education materials and encouraged all providers to initiate discussions regarding generic substitution during routine consultations. The evidence is unequivocal: for the vast majority of medications, generic formulations represent a clinically equivalent, cost-effective option that aligns with both ethical and fiscal responsibility in healthcare delivery.