When a patient is on a medication with a narrow therapeutic index-like digoxin, lithium, or vancomycin-getting the dose right isn’t just important. It’s life-or-death. Too little, and the drug doesn’t work. Too much, and it can cause toxicity, organ damage, or even death. That’s why medication monitoring isn’t optional. It’s a critical safety step. But here’s the problem: even if a lab runs the test, you can’t assume the result is accurate unless the lab has properly verified or validated the test. And if the test isn’t reliable, your follow-up decisions could be wrong. This guide cuts through the noise and shows you exactly how to confirm that monitoring labs are doing their job-and how to use those results safely.
What’s the Difference Between Verification and Validation?
Not all lab tests are created equal. If a lab uses a test kit made by Roche, Abbott, or Siemens that’s already been cleared by the FDA, they’re doing verification. That means they’re checking whether the test works the way the manufacturer says it does on their own equipment. They test precision, accuracy, and whether other substances in the blood interfere with the result. If the lab makes its own test-like for a rare metabolite of clozapine or a new biologic drug-that’s validation. Validation is far more complex. It requires proving the test works from scratch: finding the lowest level it can detect, checking if it’s accurate across the full range of expected concentrations, and testing for interference from dozens of possible substances. Validation can take months. Verification takes weeks. Why does this matter to you? Because labs that skip verification on FDA-cleared tests are cutting corners. A 2023 CAP survey found that 36% of labs didn’t properly verify the lower limit of quantitation for narrow therapeutic index drugs. That means they might miss when a patient’s level is just below the therapeutic range. For a patient on digoxin, that could mean they’re not getting enough medication-and their heart failure is worsening without anyone knowing.The 9-Step Process Labs Must Follow
Every lab that does therapeutic drug monitoring should follow a clear, documented process. If they don’t, their results shouldn’t be trusted. Here’s what a proper verification or validation looks like:- Plan it out - The lab writes a formal plan listing what they’re testing, which guidelines they’re following (CLSI EP15-A3 or APHL toolkit), and what acceptance criteria they’ll use.
- Get approval - The lab director must sign off before any testing begins. This isn’t a formality. It’s a legal requirement under CLIA.
- Run the tests - For verification, they run at least 20 replicates over five days to check precision. They test with reference materials to check bias. They spike samples with common interfering drugs (like carbamazepine or phenytoin) to see if results get skewed.
- Analyze the data - They use statistical tools to check if precision is within 1/4 of the total allowable error. For vancomycin, that means their results must be within ±15%. For digoxin, it’s ±10%.
- Fix problems - If results don’t meet criteria, they troubleshoot. Maybe the instrument needs recalibration. Maybe the reagents are expired. Maybe the interference testing missed something.
- Write the report - A full summary of all data, deviations, and conclusions. This document must be kept for at least two years.
- Create SOPs - Standard Operating Procedures for how the test is performed daily. Everyone in the lab must be trained on them.
- Final approval - The lab director reviews everything one last time and signs off.
- Start testing patients - Only after all steps are done.
If a lab skips even one of these steps, their results are unreliable. You don’t need to be a lab scientist to ask: “Did you verify this test? Can I see the documentation?”
What to Ask the Lab Before Relying on Results
You don’t have to be an expert to spot red flags. Here’s what to ask when you’re unsure about a lab’s results:- “Is this an FDA-cleared test or a lab-developed test?” - If it’s lab-developed, ask if they’ve validated it per CLSI or APHL standards.
- “What’s the total allowable error for this test?” - For lithium, it’s 10%. For tacrolimus, it’s 15%. If they don’t know, that’s a problem.
- “Did you test for interference from common drugs?” - For carbamazepine, cross-reactivity with its metabolites can cause false highs. For digoxin, antibodies from recent immunoglobulin therapy can cause false lows.
- “What’s your lower limit of quantitation?” - If it’s higher than the therapeutic range, you can’t tell if the patient is underdosed.
- “Do you report measurement uncertainty?” - Reputable labs now include this. It tells you how confident you can be in the number.
One provider in Ohio recently prescribed a higher dose of vancomycin because the lab reported a level of 18 mcg/mL. The patient developed acute kidney injury. When the provider asked for the verification report, the lab admitted they never tested linearity above 70 mcg/mL. The patient’s true level was 82 mcg/mL. The test couldn’t measure it. That’s not a lab error. That’s a failure of verification.

How to Spot a Lab That’s Cutting Corners
Some labs are under pressure to turn results around fast. Some are understaffed. Some just don’t care. Here are signs a lab isn’t doing verification right:- They won’t share documentation - If they say “it’s proprietary” or “we don’t keep it,” walk away.
- Results are inconsistent - If the same patient’s level jumps from 1.2 to 2.8 ng/mL on digoxin with no change in dose, that’s not biology. That’s bad testing.
- The same test comes back from different labs with wildly different values - That’s a red flag. One lab might be verifying properly. The other isn’t.
- They don’t use reference materials - You can’t check accuracy without them. If they say “we just run the kit,” they’re not verifying.
A 2022 study in Clinical Chemistry and Laboratory Medicine found that labs following ISO 15189 standards had 47% fewer medication errors. That’s not a small difference. That’s the difference between a patient recovering and a patient ending up in the ICU.
What Happens When Labs Get It Wrong
The consequences aren’t theoretical. In 2021, the FDA’s MAUDE database recorded a case where a lab’s digoxin test didn’t account for antibody interference. Twenty-three patients received incorrect doses. One died. Another needed emergency dialysis. In another case, a transplant center used a tacrolimus test that hadn’t been verified for cross-reactivity with metabolites. They thought their patient’s level was safe. It wasn’t. The patient rejected the new kidney. The lab had skipped testing for 12 key metabolites because “the manufacturer said it was fine.” The manufacturer’s claims were incomplete. The lab didn’t verify. These aren’t rare. The Institute of Medicine estimates 7,000-9,000 deaths per year in the U.S. are caused by medication errors. A significant portion of those come from inaccurate monitoring.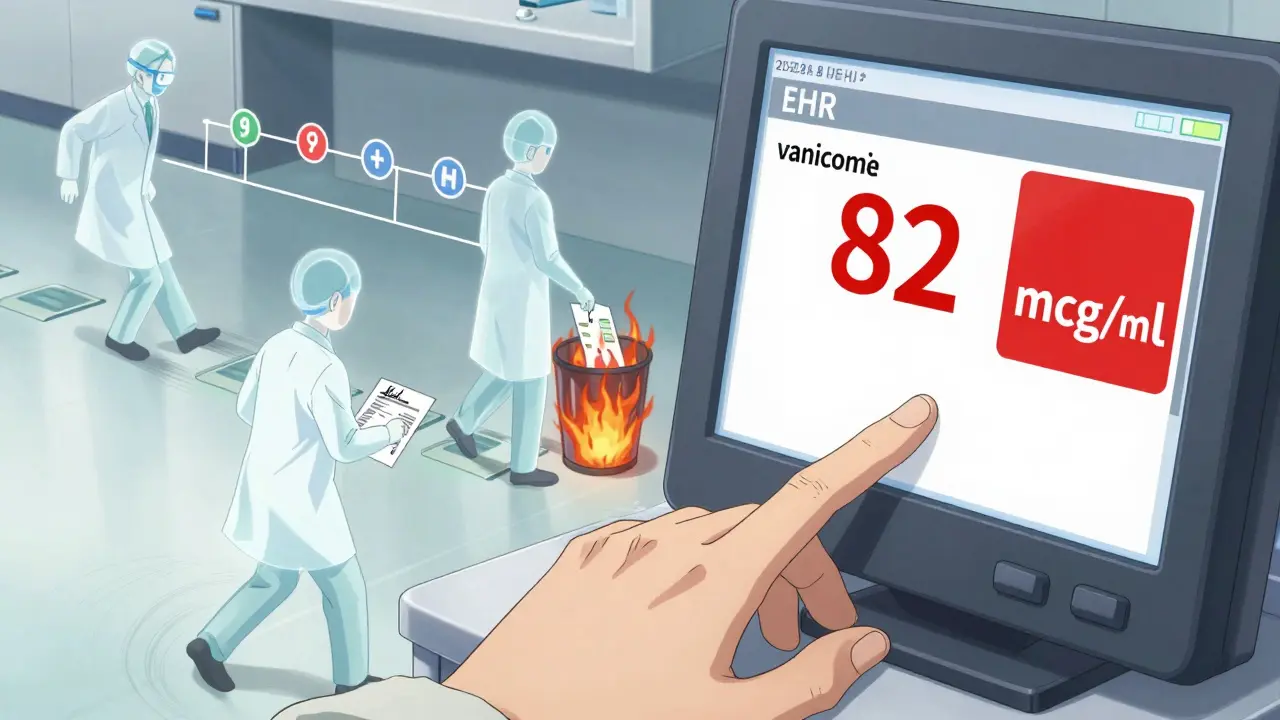
What You Can Do Today
You don’t need to run a lab. But you do need to protect your patients. Here’s what you can do right now:- Ask your lab for their verification documentation - Not just a phone call. A written summary. If they refuse, find a new lab.
- Compare results across labs - If you’re sending the same patient to two different labs and getting different numbers, investigate why.
- Use EHR alerts - Many hospitals now have systems that flag when a drug level is outside the therapeutic range. But if the lab’s test is flawed, the alert is useless. Make sure the lab is verified first.
- Train your team - Nurses, pharmacists, and PAs should understand that a lab result isn’t gospel. It’s only as good as the process behind it.
- Support labs that do it right - If you know a lab that follows APHL or CLSI guidelines, keep using them. Reward quality.
The bottom line: your job isn’t done when you order the test. Your job is done when you know the result is accurate. That means asking questions. That means holding labs accountable. That means refusing to accept results from labs that won’t prove their tests work.
What’s Changing in 2025
The FDA is tightening rules. The VALID Act proposal would require all lab-developed tests for medication monitoring to meet the same standards as commercial kits. That’s good news. It means fewer labs will be able to cut corners. Also, more labs are moving toward integrated EHR systems that auto-flag low or high levels. But those systems only work if the underlying test is verified. A flawed test with a fancy alert is still a flawed test. The trend is clear: precision medicine depends on precision labs. If you’re prescribing complex medications, you can’t afford to guess. You need proof.What’s the difference between verification and validation in medication monitoring?
Verification is when a lab confirms that an FDA-cleared test performs as the manufacturer claims. It’s faster and cheaper, taking about 80 hours and $2,500-$5,000. Validation is when a lab builds and tests its own method-like for rare drugs with no commercial kit. It’s more complex, taking 120+ hours and $7,500-$15,000. Both are required under CLIA, but they’re not interchangeable.
Which medications need the strictest monitoring?
Medications with a narrow therapeutic index need the tightest controls. These include digoxin (target range: 0.5-2.0 ng/mL), lithium (0.6-1.0 mmol/L), vancomycin (15-20 mcg/mL), and tacrolimus (5-15 ng/mL). For these drugs, even a 10-15% error in measurement can lead to toxicity or treatment failure. Labs must verify total error ≤10-15% depending on the drug.
Can I trust a lab result if the patient seems fine?
No. Patients often don’t show symptoms until levels are dangerously high or low. A patient on digoxin might feel fine with a level of 3.5 ng/mL-well above the toxic threshold. That’s why labs must verify the lower and upper limits of quantitation. If they don’t, you’re relying on luck, not science.
What should I do if a lab won’t provide verification documents?
Find a different lab. A lab that won’t share verification data is not following CLIA regulations. You’re putting your patients at risk by using their results. Ask for the APHL verification worksheet or CLSI EP15-A3 documentation. If they can’t produce it, switch to a lab that does.
Are home or point-of-care tests reliable for medication monitoring?
Most home or point-of-care tests for medications like digoxin or lithium are not FDA-cleared for clinical decision-making. Even if they give a number, they haven’t undergone the rigorous verification required for therapeutic use. Relying on them can lead to dangerous dosing errors. Always use lab-based testing with verified protocols for critical medications.
Jody Patrick
December 17, 2025 AT 07:38This is why American labs need to stop cutting corners. If you can’t verify a test, don’t run it. Period. Patients aren’t guinea pigs.
Radhika M
December 18, 2025 AT 16:46Very clear guide! I work in a small clinic in India and we send samples abroad. Now I know exactly what to ask before trusting any report. Thank you!
Philippa Skiadopoulou
December 20, 2025 AT 09:20The distinction between verification and validation is fundamental. Yet too many clinicians assume all lab results are equally reliable. This post correctly emphasizes accountability. A necessary correction to clinical complacency.
Pawan Chaudhary
December 22, 2025 AT 01:55Love this! So many of us just trust the numbers without asking how they got there. This is a wake-up call-and a really practical one. Keep sharing stuff like this!
Anna Giakoumakatou
December 23, 2025 AT 23:17Oh wow. Another ‘clinical guide’ that treats physicians like children who can’t think for themselves. Of course labs must verify. Do you really think we’re all idiots who just blindly trust machines? This reads like a compliance pamphlet disguised as medical wisdom.
Sam Clark
December 24, 2025 AT 04:40While the tone of this post may appear overly prescriptive, its underlying message is both clinically sound and ethically imperative. The responsibility to ensure diagnostic integrity rests not solely with laboratories but with the prescribing clinician. We must institutionalize verification as a non-negotiable standard of care.
Chris Van Horn
December 25, 2025 AT 20:13Let me guess-this is the same guy who thinks ‘CLIA’ is a yoga pose. You people act like lab techs are magicians who wave wands and poof-accurate numbers appear. Newsflash: most labs are underfunded, understaffed, and overworked. Instead of throwing around ‘verification’ like a magic spell, maybe help them fix the system? Or are you just here to flex your medical superiority?
Peter Ronai
December 26, 2025 AT 09:38HA! You think this is the only place where labs cut corners? Try reading the FDA’s 2023 whistleblower reports. Half the ‘validated’ tests in academic hospitals were done by interns who didn’t even know what ‘linearity’ meant. And you’re shocked? This isn’t negligence-it’s systemic rot. We need to burn the whole system down and start over.
Steven Lavoie
December 28, 2025 AT 04:35As someone who has worked in labs across five countries, I’ve seen how cultural attitudes toward quality control vary wildly. In the U.S., there’s pressure to rush. In Germany, it’s bureaucracy. In India, it’s often resource limits. But the science doesn’t change. Verification isn’t optional-it’s the foundation. This guide should be required reading for every prescriber, everywhere.
Anu radha
December 29, 2025 AT 14:53I’m a nurse in a rural clinic. We don’t have fancy labs nearby. But now I know to ask: ‘Can you show me the paper that says your test works?’ That’s all. Just one question. It changes everything.
Salome Perez
December 30, 2025 AT 20:08This is the kind of content that reminds me why I love medicine-not the glamour, but the quiet, relentless pursuit of truth. Thank you for writing this with such clarity and courage. The patients you protect with these questions? They’ll never know your name. But they’ll live longer because of it.
Evelyn Vélez Mejía
December 30, 2025 AT 20:09Verification and validation are not procedural checkboxes-they are epistemological commitments. The clinical act of prescribing is inseparable from the epistemic reliability of the data upon which it rests. To accept unverified results is to surrender reason to algorithmic mysticism. The physician, in this context, becomes not a healer, but a conduit for institutional negligence.
Meghan O'Shaughnessy
December 31, 2025 AT 09:08Interesting. I’ve been using the same lab for five years. Just called them. They sent me the verification report. Turns out they skipped interference testing for phenytoin. I’m switching labs tomorrow.