When you walk into a doctor’s office, emergency room, or pharmacy, your medical records should tell the story of your health - clearly, accurately, and without guesswork. One of the most critical parts of that story? Your drug allergies. A simple mistake here - like writing ‘penicillin allergy’ without details - could lead to a life-threatening reaction. Yet, studies show that nearly 40% of recorded drug allergies are vague, outdated, or outright wrong. If you’ve ever been told you’re allergic to a drug but never had a real reaction, or if your records just say ‘allergic to sulfa’ without saying which drug or what happened - you’re not alone. And you’re at risk.
Why Exact Details Matter More Than You Think
Let’s say you tell your doctor, ‘I’m allergic to penicillin.’ That’s fine - but it’s not enough. Penicillin is a family of drugs. If your reaction was a rash after taking amoxicillin 15 years ago, that doesn’t mean you’re allergic to ampicillin, cephalexin, or even azithromycin. Yet, most hospitals will avoid all penicillin-related drugs if you just say ‘penicillin allergy.’ That means you might get a less effective, more expensive, or more toxic antibiotic - just because the record lacks detail. The Institute of Medicine found that poor allergy documentation contributes to over 1.3 million injuries and 7,000 deaths every year in the U.S. alone. That’s not a hypothetical risk. It’s happening right now. And it’s often because people don’t know what to record - or how to record it.What Exactly Should You Write Down?
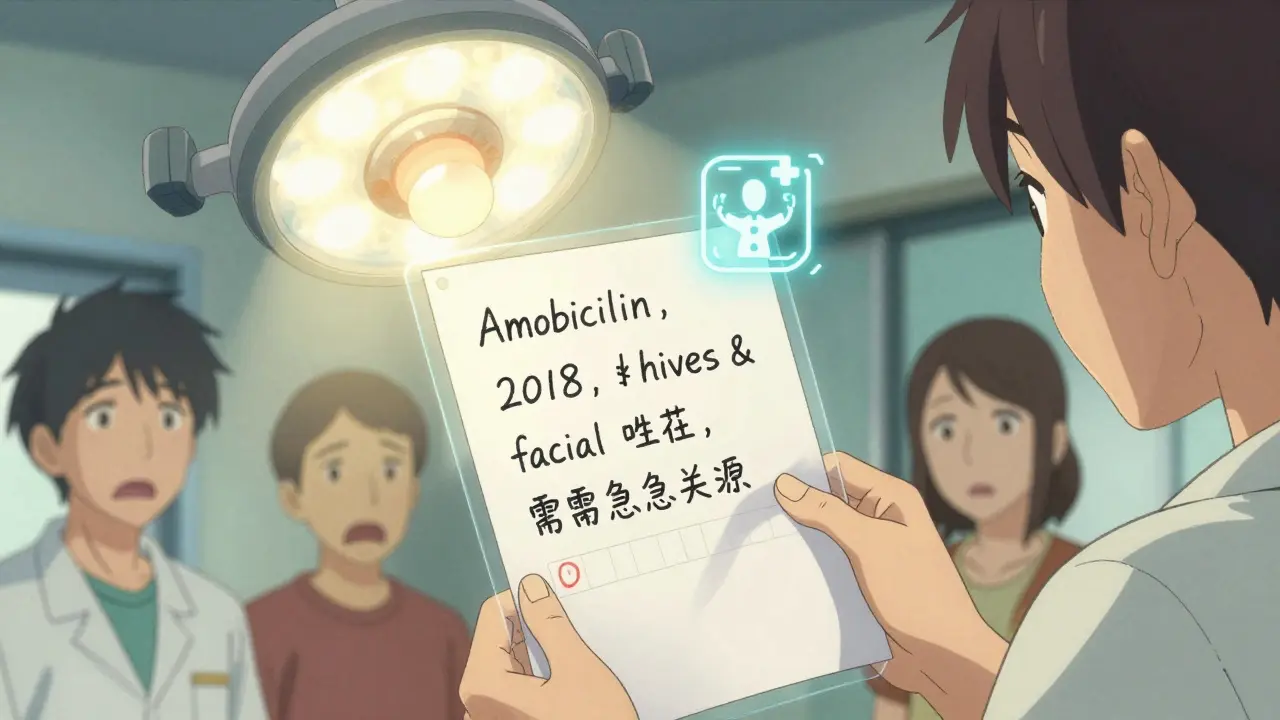
Your medical record isn’t just a list of drugs you’ve taken. It’s a safety tool. And for allergies, it needs four things:- The exact drug name - use the generic name, not the brand. Say ‘amoxicillin,’ not ‘Amoxil.’ Say ‘sulfamethoxazole,’ not ‘Bactrim’ or ‘sulfa.’ Brand names vary by country and can be misleading.
- The reaction - what actually happened? Did you get a rash? Swelling? Trouble breathing? Nausea? Hives? Anaphylaxis? Be specific.
- How severe it was - mild, moderate, or life-threatening? Did you need epinephrine? Hospitalization?
- When it happened - years ago? Last month? Did you take the drug again and react again?
Example of good documentation: ‘Amoxicillin, 2018. Developed hives and facial swelling within 30 minutes of taking the pill. Required antihistamines and emergency care. No reaction since.’
Example of bad documentation: ‘Allergic to penicillin.’ - This tells doctors nothing useful. It just makes them avoid a whole class of safe drugs.
Don’t Assume You’re Still Allergic
Here’s the shocking truth: 90% of people who think they’re allergic to penicillin aren’t. Not anymore. Not ever. Many reactions were misdiagnosed - maybe it was a viral rash, or a side effect, not a true allergy. Over time, allergies fade. The immune system forgets. A 2017 JAMA Internal Medicine study tested over 300 patients who claimed penicillin allergy. After skin testing, 92% of them could safely take penicillin again. That means thousands of people are being denied the best, cheapest, and safest antibiotics - simply because their records haven’t been updated. If you had a reaction years ago - especially as a child - talk to your doctor about getting tested. A simple skin test or oral challenge can clear your record and open up better treatment options.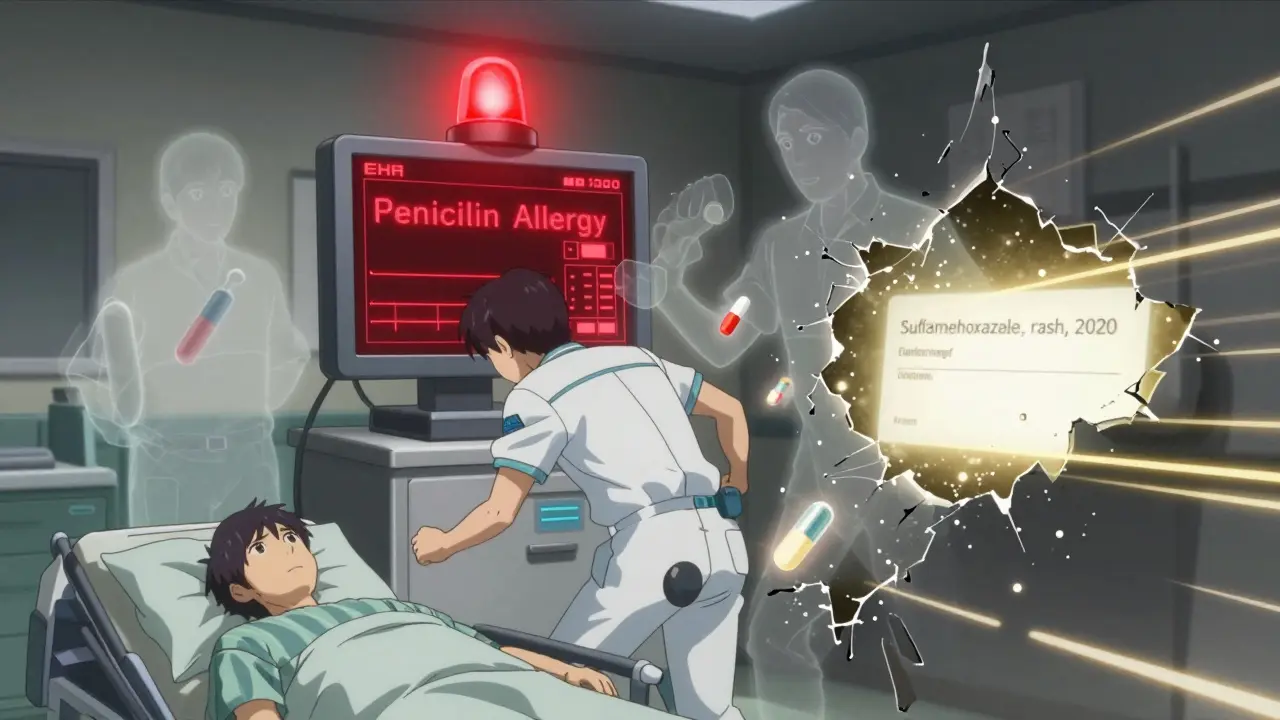
How to Make Sure Your Records Are Right
You’re the most important person in your medical team. No one else knows your body like you do. Here’s how to take control:- Before every appointment, review your allergy list. Ask your doctor or nurse: ‘Can we go over my drug allergies together?’
- Bring a written list - even if your doctor has it. Write down the drug, reaction, severity, and date. Keep it in your phone or wallet.
- Ask if your record says ‘No Known Drug Allergies’ (NKDA). If it doesn’t say that, and you truly have no allergies, ask them to add it. Empty records are dangerous too - doctors assume you might be allergic if it’s not stated.
- If you’ve had a reaction to a drug, ask your doctor to document the reaction in your EHR using the exact terms: ‘hives,’ ‘anaphylaxis,’ ‘angioedema,’ ‘Stevens-Johnson syndrome.’ These are clinical terms that trigger alerts in hospital systems.
- Ask if your clinic uses a standardized tool like the Drug Allergy History Tool (DAHT). It’s a short questionnaire that helps patients recall details they might forget.
What Happens If You Don’t Document Correctly?
Imagine you’re rushed to the ER with a severe infection. The doctor sees ‘allergic to penicillin’ and reaches for a stronger, broader-spectrum antibiotic. That drug costs more. It’s harder on your gut. It increases your risk of C. diff infection. And it might not even work as well. Or worse - the doctor misses the allergy entirely because it’s buried in a note, not flagged. You get the drug. You go into anaphylactic shock. That’s not rare. The Joint Commission calls incomplete allergy documentation a ‘sentinel event’ - one of the top causes of preventable harm in hospitals. Even small mistakes add up. A 2019 study in the Journal of the American Medical Informatics Association found that 6.5% of all medication errors were tied to incorrect or missing allergy info. That’s over 2 million errors a year in the U.S. alone.How Technology Can Help - and Hurt
Most clinics now use electronic health records (EHRs) like Epic, Cerner, or Meditech. These systems are supposed to make things safer. They flag allergies when a doctor tries to prescribe a drug. But here’s the catch: they only work if the data is accurate. If your record says ‘penicillin allergy’ with no details, the system will block every penicillin-like drug - even ones you’ve taken safely for years. If it says ‘allergic to sulfa’ without naming the drug, it might block sulfamethoxazole-trimethoprim (Bactrim), but not sulfasalazine (used for arthritis), even though those are completely different chemicals. The good news? Systems are getting smarter. Since 2023, all certified EHRs in the U.S. must use the FHIR standard - which lets your allergy data travel safely between hospitals, pharmacies, and even your phone. If you use a health app like Apple Health or MyChart, you can now update your allergy list yourself. But only if you know what to put in.What You Can Do Today
You don’t need to wait for your next appointment. Start now:- Open your patient portal. Look for your allergy list. Is it specific? Does it say ‘ampicillin’ or just ‘penicillin’? Does it describe the reaction?
- If it’s vague or missing, send a secure message to your doctor: ‘I’d like to update my drug allergy record. Can we schedule a 10-minute call to clarify?’
- If you’ve never been tested for a suspected allergy - especially penicillin - ask about it. Testing is safe, quick, and often covered by insurance.
- Keep a printed copy of your updated list in your wallet or phone. Share it with any new provider.
There’s no such thing as over-documenting a drug allergy. Under-documenting? That’s where the danger lives.
Final Thought: Your Record Is Your Shield
Your medical record isn’t just paperwork. It’s your shield. It’s what keeps you safe when you can’t speak for yourself - during surgery, in the ER, in the middle of the night. If your allergy info is vague, your shield has holes. If it’s detailed, accurate, and up to date, it’s bulletproof.Take 10 minutes today. Review your records. Update them. Ask questions. You’re not just filling out a form. You’re saving your own life.
What if I think I’m allergic to a drug but I’m not sure?
Don’t assume. Many people label side effects - like nausea or a mild rash - as allergies. True drug allergies involve the immune system and often include symptoms like hives, swelling, trouble breathing, or anaphylaxis. If you’re unsure, talk to your doctor. You may be able to get a skin test or oral challenge to confirm whether it’s a real allergy. Up to 90% of people who think they’re allergic to penicillin turn out not to be.
Can I update my drug allergy list myself?
Yes, if your provider uses a patient portal like MyChart, Apple Health, or Epic’s MyChart. Most allow you to add or edit your allergy list directly. But always confirm with your doctor afterward. Even if you update it yourself, your provider needs to review and approve it to ensure it’s coded correctly in the system. Don’t rely on your input alone - get it verified.
Why does my doctor ask about allergies every time I visit?
Because allergies can change. You might have outgrown one. Or developed a new one. Also, rules require that your allergy list be confirmed at every new visit or admission - even if it’s unchanged. Saying ‘No Known Drug Allergies’ (NKDA) is just as important as listing an allergy. If it’s not documented, providers assume you might have one.
What’s the difference between a drug allergy and a side effect?
A side effect is a known, expected reaction - like drowsiness from antihistamines or stomach upset from antibiotics. A drug allergy is an immune system response. It’s unpredictable and can get worse with each exposure. Signs include hives, swelling, wheezing, or low blood pressure. If you’re not sure, describe the reaction to your doctor. They can help you tell the difference.
Does my pharmacy know my drug allergies?
Sometimes. Pharmacies pull data from your insurance or EHR, but it’s not always accurate or complete. Always tell your pharmacist about your allergies when picking up a new prescription - even if you think they already know. They’re your last line of defense before you take the medication.
Christina Widodo
January 13, 2026 AT 05:02My mom had a rash after amoxicillin when she was 8, and they just labeled her 'penicillin allergic' for 40 years. Last year, she got tested-turned out she’s fine. Now she takes amoxicillin like it’s candy. Why do we still treat allergy labels like life sentences?
laura manning
January 14, 2026 AT 14:54The clinical precision required in documenting drug allergies is non-negotiable. The absence of specificity-such as failing to distinguish between sulfamethoxazole and sulfasalazine-constitutes a critical failure in pharmacovigilance. Standardized terminology, per HL7 FHIR guidelines, must be enforced universally; otherwise, decision-support systems remain fundamentally compromised. This is not a suggestion-it is a patient-safety imperative.
Alice Elanora Shepherd
January 14, 2026 AT 22:03I’ve been a nurse for 18 years, and I’ve seen too many patients avoid life-saving antibiotics because their records just say 'allergic to penicillin.' I always ask patients to describe the reaction-was it a rash? Swelling? Did they feel like they were dying? That’s the difference between a harmless side effect and a real allergy. If you’re not sure, write it down anyway-then ask your doctor to help you clarify it. It’s not extra work-it’s your safety.
Lawrence Jung
January 15, 2026 AT 13:04People treat allergies like they’re tattoos when they’re more like receipts-expired ones at that. You got a rash at 12? Cool. But your immune system isn’t stuck in 2003. Stop letting doctors treat you like a walking error log. Get tested. Stop being a liability to yourself and the system
Windie Wilson
January 16, 2026 AT 06:24Oh wow, so now I have to become a pharmacologist just to not die in the ER? Thanks, America. My chart says 'penicillin allergy' and I'm fine with that. Let the robots figure it out. I paid for my insurance so I don’t have to be my own medical scribe.
Cassie Widders
January 17, 2026 AT 21:23I used to just say 'sulfa allergy' until my pharmacist asked what drug exactly. Turns out it was Bactrim-I never reacted to sulfasalazine. Now I write it all down. Simple. Helps everyone.
Amanda Eichstaedt
January 19, 2026 AT 21:17My grandma had a reaction to penicillin when she was 10. She’s 82 now. Last year, her allergist did a scratch test. She’s fine. She’s been on penicillin for pneumonia twice since. She says, 'Why did I waste 70 years avoiding something that never hurt me?' This isn’t just about medicine-it’s about freeing yourself from old fears.
Konika Choudhury
January 21, 2026 AT 17:19Why should I waste time writing down every little thing when my doctor is paid to know this stuff? In India we trust our doctors not to make mistakes. You Americans overthink everything. Just take the pill and stop making paperwork
Abner San Diego
January 23, 2026 AT 04:56Look, I’ve been to 12 different doctors in the last 5 years. Every time they ask about allergies, I say 'penicillin' and move on. If they can’t figure out which one I mean, that’s their problem. I’m not rewriting my medical history every time I get a cold. I’ve got a job. I’ve got kids. I don’t have time to be a medical data entry clerk.