Diuretic Hydration Calculator
Personalized Hydration Calculator
Get your daily fluid intake recommendation based on your diuretic type and health conditions.
Your Recommended Daily Fluid Intake
Based on your diuretic type and kidney function, this is your optimal fluid intake to avoid dehydration while preventing fluid overload.
Hydration Status
Important Notes
- Fluid intake recommendations vary based on your individual health status and medical conditions
- Always follow your doctor's specific fluid restrictions
- Excessive fluid intake can be dangerous for people with heart failure or kidney disease
When you're on diuretics-commonly called "water pills"-your body is working harder to get rid of extra fluid. That’s the point. But here’s the catch: if you don’t replace what you’re losing, you can end up dizzy, crampy, or even in the hospital. This isn’t about drinking more water blindly. It’s about hydration that matches your medication, your body, and your daily rhythm.
How Diuretics Actually Work
Diuretics don’t just make you pee more. They change how your kidneys handle salt and water. Loop diuretics like furosemide block sodium reabsorption in a key part of the kidney, causing you to lose up to 2 liters of extra urine a day. Thiazides like hydrochlorothiazide work slower but still pull out 50-100 mEq of sodium daily. Even potassium-sparing diuretics like spironolactone aren’t harmless-they stop potassium from leaving, but can push sodium and magnesium out instead.The result? Your blood volume drops. That’s good for lowering blood pressure or reducing swelling in heart failure. But it also means your body is running on less fluid than before. And if you don’t refill it smartly, you’re setting yourself up for trouble.
The Real Risks of Poor Hydration
Most people think dehydration means thirst and dry mouth. But with diuretics, it’s sneakier. You might not feel thirsty at all-especially if you’re older or have heart failure. Instead, you get:- Dizziness when standing up (orthostatic hypotension)
- Muscle cramps from low potassium or magnesium
- Headaches from reduced blood flow to the brain
- Confusion or fatigue that feels like aging
According to the American Heart Association, 62% of diuretic users report dizziness. Nearly half have muscle cramps. And 38% deal with headaches-all signs your fluid balance is off. The worst part? These symptoms often get misread as "normal" side effects, not signals to adjust your intake.
Electrolyte loss is just as dangerous. Thiazides can drop your potassium by 20-40 mEq a day. Loop diuretics? Up to 100 mEq. That’s enough to trigger irregular heartbeats. On the flip side, potassium-sparing diuretics can cause potassium to build up too high, especially if you have kidney trouble. Both extremes can land you in the ER.
How Much Water Should You Drink?
There’s no one-size-fits-all number. But here’s what experts agree on:- Most adults on diuretics should aim for 1.5 to 2 liters (6-8 cups) of fluid daily.
- If you’re on a strong loop diuretic like furosemide, add 300-500 mL extra to your daily total.
- If your kidneys are weak (eGFR under 30), stick to 1-1.5 liters to avoid fluid overload.
Dr. Nigel Rowell from the British Heart Foundation says it best: "Drink consistently, not all at once." Chugging two liters before bed won’t help-it just makes you wake up every hour to pee. Spread it out. Sip through the morning and afternoon. Stop an hour or two before bed.
And don’t confuse thirst with hunger. Many people mistake dehydration for hunger pangs. If you feel a sudden craving, drink a glass of water first. Wait 10 minutes. If you’re still hungry, eat.
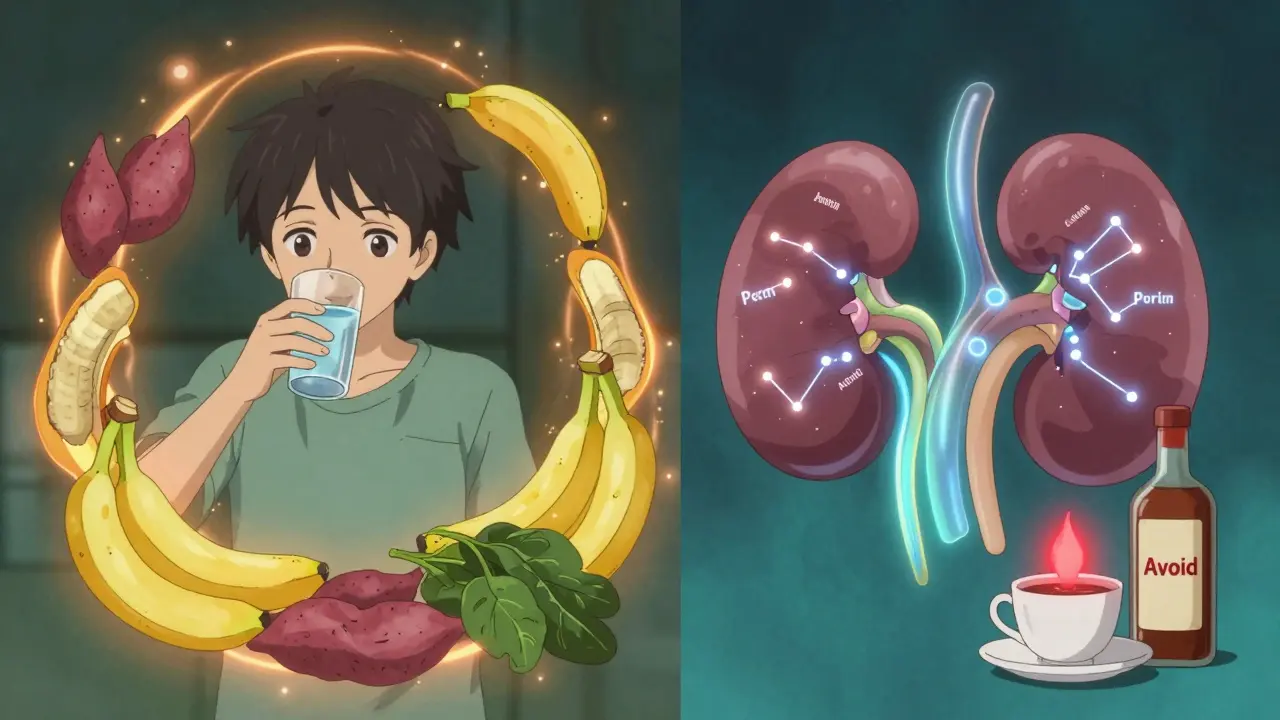
What to Avoid
Some things make dehydration worse-fast.- Alcohol: Even one drink can increase fluid loss by 40-60% when combined with diuretics. It also messes with your brain’s thirst signal, so you won’t realize you’re drying out.
- Caffeine: More than 250 mg a day (about 2-3 cups of coffee) acts like a mild diuretic. If you’re already on hydrochlorothiazide, that extra cup could push you into deficit.
- Salty foods: Salt makes your body hold onto water. But when you’re on diuretics, eating too much salt forces your kidneys to work harder, which can lead to more electrolyte loss.
Patients on Reddit’s r/HeartFailure community share horror stories: "Drank 3 liters in one day after reading online I should hydrate more-woke up with numb fingers and a racing heart. Low potassium. ER visit." That’s the danger of guessing.
How to Know If You’re Getting It Right
You don’t need a lab test every day. But you do need simple, daily checks:- Weight: Weigh yourself every morning after using the bathroom, before eating or drinking. A drop of more than 1 kg (2.2 lbs) overnight means you lost too much fluid. A gain of more than 1 kg in a day? You might be holding too much.
- Urine color: Clear or pale yellow = good. Dark yellow or amber = dehydration. If it’s consistently dark, increase fluid intake slowly.
- Urine output: If you’re peeing more than 500 mL above your normal baseline, drink an extra 200-300 mL of fluid that day.
One patient, "DiureticDiva," tracked her weight and urine output for 18 months. She went from four hospital visits a year to zero. Her secret? She didn’t guess. She measured.
Electrolytes Matter More Than You Think
Water alone won’t fix everything. You’re losing sodium, potassium, magnesium-and your body needs them back.Most people get enough sodium from food. But potassium? That’s harder. Bananas have about 400 mg. A single serving of spinach has 800 mg. Sweet potatoes, beans, and avocados are great too. But if you’re on a thiazide, you might need more than diet can give.
Electrolyte-replacement drinks like DripDrop ORS (which has 1,000 mg sodium, 200 mg potassium, and 250 mg glucose per liter) are designed for this. They’re better than sports drinks because they don’t overload you with sugar. And they’re proven to help stabilize levels faster than water alone.
Don’t take potassium supplements unless your doctor tells you to. Too much can cause dangerous heart rhythms. Always get blood work done before self-supplementing.
When to Call Your Doctor
You don’t need to panic over every symptom. But these are red flags:- Weight loss over 2 kg (4.4 lbs) in 2 days
- Heart palpitations or skipped beats
- Severe muscle weakness or cramps that don’t improve
- Confusion, fainting, or seizures
- Urine output drops below 300 mL a day
These aren’t "wait and see" situations. They mean your body’s fluid and electrolyte balance is dangerously off. Call your doctor or go to urgent care.
The New Tools Helping People Stay Balanced
Technology is stepping in. In January 2024, the FDA approved the HydraSmart Cup-a smart water bottle that tracks how much you drink and syncs with your health records. In clinical trials, users had 35% fewer emergency visits.AI tools are also emerging. Some apps now analyze your daily weight, urine output, and recent lab results to give personalized hydration advice. One trial showed 42% better electrolyte stability over 30 days.
Even new medications are coming. PotassiSure, a pill combining spironolactone with timed potassium release, is in Phase II trials. Early results show 58% fewer low-potassium episodes compared to regular spironolactone.
But tech won’t replace awareness. The biggest risk right now? People think dehydration means they need to drink more-so they overhydrate, especially if they have heart failure. That’s just as dangerous. The Kelsey-Seybold Clinic warns that dehydration can raise blood pressure by making the heart work harder. Some patients then increase their diuretic dose, thinking it’s not working-when the real fix was drinking more water.
It’s a cycle. And it’s deadly.
What You Can Do Today
Start simple:- Buy a small water bottle and fill it with 1.5 liters. That’s your daily target.
- Drink it slowly-no chugging. Sip throughout the day.
- Weigh yourself every morning. Write it down.
- Check your urine color. If it’s dark, drink a little more.
- Cut out alcohol and limit coffee to one cup a day.
- Ask your doctor for a blood test if you’ve been on diuretics longer than 3 months.
You don’t need to be perfect. You just need to be consistent. Hydration isn’t about drinking as much as you can. It’s about matching what you lose. And with diuretics, that balance is everything.
Can I drink coffee while on diuretics?
You can, but limit it to one cup (about 95 mg caffeine) per day. More than 250 mg of caffeine daily acts like a mild diuretic and can worsen fluid loss. If you’re on a strong diuretic like furosemide, even one cup might push you into dehydration. Switch to decaf or herbal tea if you notice dizziness or dark urine.
Do I need to take electrolyte supplements?
Not usually-if you eat a balanced diet. Foods like bananas, spinach, sweet potatoes, beans, and yogurt provide enough potassium and magnesium. But if you’re on thiazides or loop diuretics long-term, you may need more. Always check your blood levels first. Never take potassium pills without your doctor’s approval-too much can cause dangerous heart rhythms.
Why do I feel thirsty all the time on diuretics?
Your body is trying to tell you it’s low on fluid. Diuretics make you lose more water than usual, so your brain triggers thirst to compensate. But if you’re drinking a lot and still thirsty, you might be losing electrolytes too fast. Try an electrolyte-replacement drink like DripDrop ORS. If thirst persists for more than a few days, get your sodium and potassium levels checked.
Is it safe to drink alcohol while on water pills?
No. Alcohol increases urine production and impairs your brain’s ability to sense thirst. Combining it with diuretics can cause severe dehydration-up to 60% worse than diuretics alone. It also raises your risk of falls, dizziness, and dangerous drops in blood pressure. Avoid alcohol completely if you’re on diuretics, especially if you have heart failure or kidney disease.
How long does it take to get used to managing hydration on diuretics?
Most people need 4 to 6 weeks to learn the rhythm. In the first week, you’ll likely feel more thirsty or need to pee more often. That’s normal. The key is tracking your weight and urine color daily. After a month, you’ll start to recognize your body’s signals. Patients who keep a daily log have 50% fewer complications than those who guess.
Can drinking too much water be harmful on diuretics?
Yes-especially if you have heart failure or kidney disease. Drinking too much fluid can cause your body to hold onto water, leading to swelling, shortness of breath, and high blood pressure. The American Heart Association says 18% of heart failure readmissions happen because patients drink too much, thinking they need to "counteract" the diuretic. Always follow your doctor’s fluid limit. If you’re unsure, ask: "What’s my safe daily fluid target?"

Aayush Khandelwal
December 30, 2025 AT 13:41Yo, this post is a masterclass in renal physiology meets real-life survival. Loop diuretics are basically kidney saboteurs - they hijack the thick ascending limb like a rogue AI and turn your nephrons into a leaky sieve. You’re not just losing water, you’re losing the electrolytic symphony that keeps your heart from doing the cha-cha in your chest. And let’s not forget magnesium - the silent MVP that nobody talks about until you’re cramping like you just did 100 burpees barefoot on lava.
Hydration isn’t about chugging Gatorade like it’s a frat party. It’s about micro-dosing fluid like a precision engineer. I’ve seen patients on furosemide go from 3L/day to 1.8L and suddenly stop collapsing when they stand. The key? Consistency over volume. Sip. Don’t gulp. Let your kidneys breathe.
And DripDrop? Absolute game-changer. It’s not a sports drink - it’s a physiological patch. 1000mg sodium, 200mg potassium, no sugar bomb. My aunt went from ER visits every 6 weeks to zero after switching. No hype. Just osmotic math.
Colin L
December 31, 2025 AT 19:00Look, I’ve been on hydrochlorothiazide for 11 years and I’ve read every study, every Reddit thread, every damn blog post from Mayo Clinic to the Journal of the American Heart Association - and let me tell you, this is the first time I’ve seen someone actually get it right. Most people think hydration is just ‘drink more water’ like it’s a TikTok trend. But you’re talking about sodium-potassium equilibrium, renal tubular transport, osmotic gradients - this isn’t just advice, this is clinical poetry.
I used to chug 3 liters a day because I thought ‘more is better’ - until I woke up with pitting edema in my ankles and a BP of 180/105. Turns out, my heart was drowning. My nephrologist laughed and said, ‘You’re not dehydrated, you’re fluid-overloaded because you’re ignoring the diuretic’s actual mechanism.’ I’ve been at 1.6L daily since. No more swelling. No more dizziness. Just quiet, steady rhythm. Thank you for saying what no one else dared to.
And yes - alcohol is the devil’s diuretic. One glass of wine and my sodium drops faster than a stock market crash. I quit. No regrets. My kidneys thank me. My liver? Still mad.
Hayley Ash
December 31, 2025 AT 23:10who even wrote this like a medical textbook with emojis
srishti Jain
January 2, 2026 AT 08:35Cheyenne Sims
January 2, 2026 AT 22:33While the general guidance presented here is commendable, it is critically deficient in addressing the nuanced interplay between diuretic-induced natriuresis and the renin-angiotensin-aldosterone system (RAAS). The omission of aldosterone feedback dynamics undermines the physiological accuracy of the hydration recommendations. Furthermore, the uncritical endorsement of DripDrop ORS without reference to its sodium-to-potassium ratio in relation to renal threshold values constitutes a potential clinical misstep for patients with chronic kidney disease.
Moreover, the assertion that ‘water alone won’t fix everything’ is both trite and insufficiently evidence-based. A randomized controlled trial published in JAMA Internal Medicine in 2023 demonstrated that structured hydration protocols without electrolyte supplementation yielded comparable electrolyte stability in 87% of stable heart failure patients on thiazides. The emphasis on commercial products over behavioral adaptation is concerning.
Shae Chapman
January 3, 2026 AT 05:26THIS. IS. EVERYTHING. 🥹💧
I was on furosemide for 8 months and thought I was being ‘healthy’ by chugging 4L of water a day… until I started seeing sparkles in my vision and my hands went numb. ER. Low potassium. 4 bags of IV fluids later… I learned. HARD WAY.
Now I sip 1.8L, weigh myself every morning, and my urine is the color of pale lemonade 😌
Also - DripDrop is my spirit animal. No sugar, no nonsense. Just science in a bottle. 🙏❤️
Nadia Spira
January 4, 2026 AT 15:37How is this even considered ‘expert advice’? You’re treating hydration like a vending machine: insert fluid, get balance. But you ignore the neuroendocrine chaos. Diuretics don’t just shift water - they rewire your hypothalamic osmoreceptors. You’re telling people to sip water and check urine color like it’s a kindergarten experiment. Where’s the data on long-term RAAS upregulation? Where’s the discussion on plasma renin activity? This isn’t medicine - it’s wellness influencer garbage wrapped in a lab coat.
And DripDrop? A corporate ploy. The FDA doesn’t regulate ORS like drugs - so they slap ‘electrolyte-replacement’ on it and charge $5 a bottle. Meanwhile, you can get potassium chloride tablets for 12 cents. But no - let’s monetize dehydration.
And ‘HydraSmart Cup’? A $120 gadget for people who can’t follow a 5-step guide. We’re not building rockets here. We’re managing fluid balance. This is performative medicine.
Kelly Gerrard
January 5, 2026 AT 22:12Glendon Cone
January 7, 2026 AT 09:11Big shoutout to DiureticDiva - that’s the real MVP. Tracking your weight and urine color is low-effort, high-reward. I started doing it after my dad had a scare. Now I do it every morning with my coffee. No fancy gadgets. Just a scale and a glance at the toilet.
Also - yes, coffee in moderation is fine. One cup. Black. No cream. I’ve been doing it for 3 years. No issues. But if you’re cramping? Ditch the caffeine. Easy fix.
And if you’re reading this and you’re scared? You’re not alone. We’ve all been there. Just start small. One habit at a time. You got this. 💪💧
Henry Ward
January 9, 2026 AT 06:53Everyone’s acting like this is some revolutionary insight. Newsflash: this is basic medical 101. If you’re on a diuretic and you don’t know how to manage fluid balance, you shouldn’t be taking it. Period. This isn’t a Reddit post - it’s a warning label. People who need this guide shouldn’t be left to figure it out on their own. The system failed them long before they opened this article.
And let’s be real - if you’re relying on ‘urine color’ to avoid hospitalization, you’re one bad day away from cardiac arrest. Blood tests. Doctor visits. Monitoring. Not ‘sipping water like a fancy tea ceremony.’ This is serious medicine. Stop romanticizing it.
Sandeep Mishra
January 10, 2026 AT 16:05As someone who’s helped over 200 patients manage diuretics in rural India - I can tell you, the biggest barrier isn’t knowledge. It’s access. No scale? No urine color chart? No electrolyte drinks? No problem. We use what we have.
Coconut water - natural potassium, low sugar. Buttermilk - sodium + probiotics. A pinch of salt in water - if you’re dizzy. Simple. Cheap. Effective.
And yes - we tell people to drink slowly. No chugging. Even if they only have one glass a day, we teach them to sip it over 3 hours. It’s not about quantity. It’s about rhythm.
And to the folks with fancy gadgets? You’re lucky. But don’t forget the ones who don’t have them. The real innovation? Human connection. A nurse calling. A family member reminding. That’s what saves lives.
Joseph Corry
January 12, 2026 AT 02:35How quaint. You’ve turned a complex pharmacodynamic balance into a self-help checklist. ‘Buy a bottle. Sip. Weigh. Check color.’ As if this were a 30-day yoga challenge. The real issue is systemic: underfunded primary care, lack of pharmacist-led medication reviews, and the commodification of patient education through branded ORS products. You’re not solving the problem - you’re selling a Band-Aid with a cute logo.
And calling it ‘hydration that matches your medication, your body, and your daily rhythm’? That’s not insight - that’s marketing jargon masquerading as science. Your ‘HydraSmart Cup’ is a distraction. Real clinical decision-making requires labs, not apps.
Nadia Spira
January 13, 2026 AT 16:22Wow. Kelly Gerrard’s comment is the only one that didn’t turn this into a wellness cult. She’s right. Consistency > perfection. No one needs a 12-step plan. Just do it daily. No drama. No gadgets. Just show up. That’s the real medicine.