When your knees ache after walking the dog, or your fingers stiffen up in the morning, it’s easy to brush it off as just getting older. But if this keeps happening, it’s not normal aging-it could be osteoarthritis (OA). This isn’t just "wear and tear." It’s a full-joint disease, where cartilage breaks down, bones rub, ligaments tighten, and inflammation creeps in. And it’s not rare. Over 32 million adults in the U.S. have it. Globally, more than half a billion people live with OA. It’s the leading cause of disability worldwide.
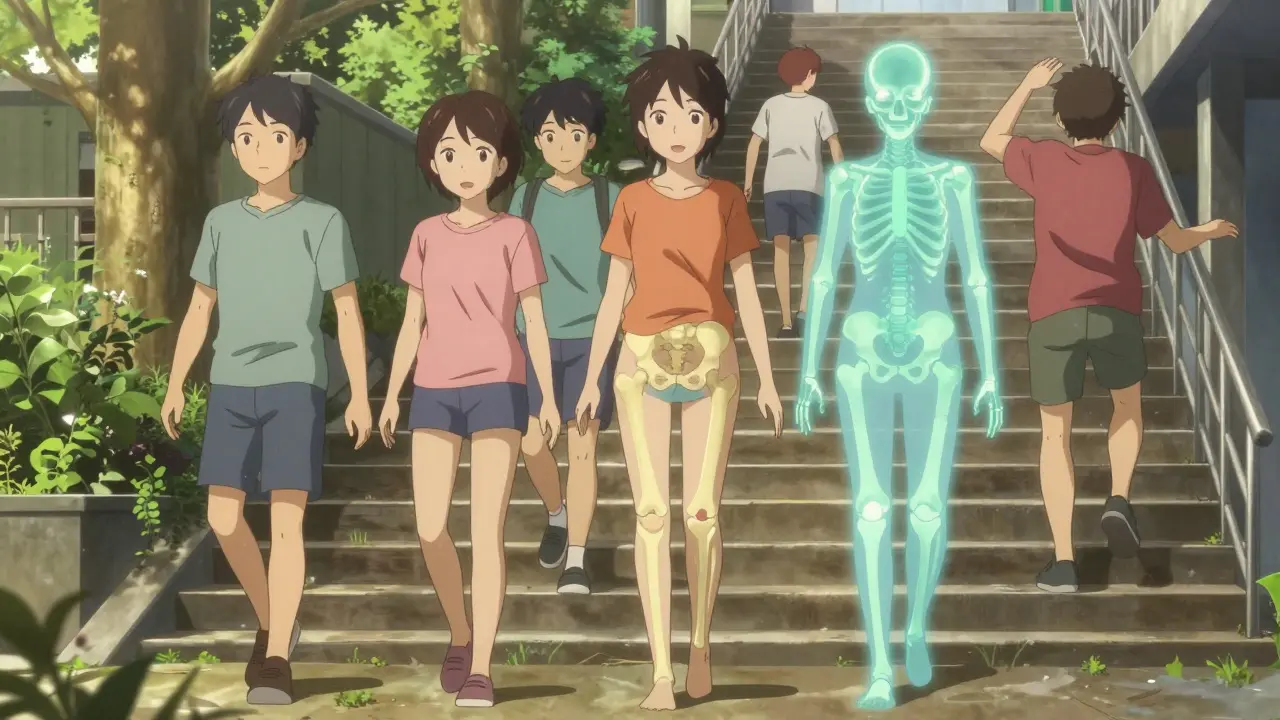
What’s Really Happening Inside Your Joint?
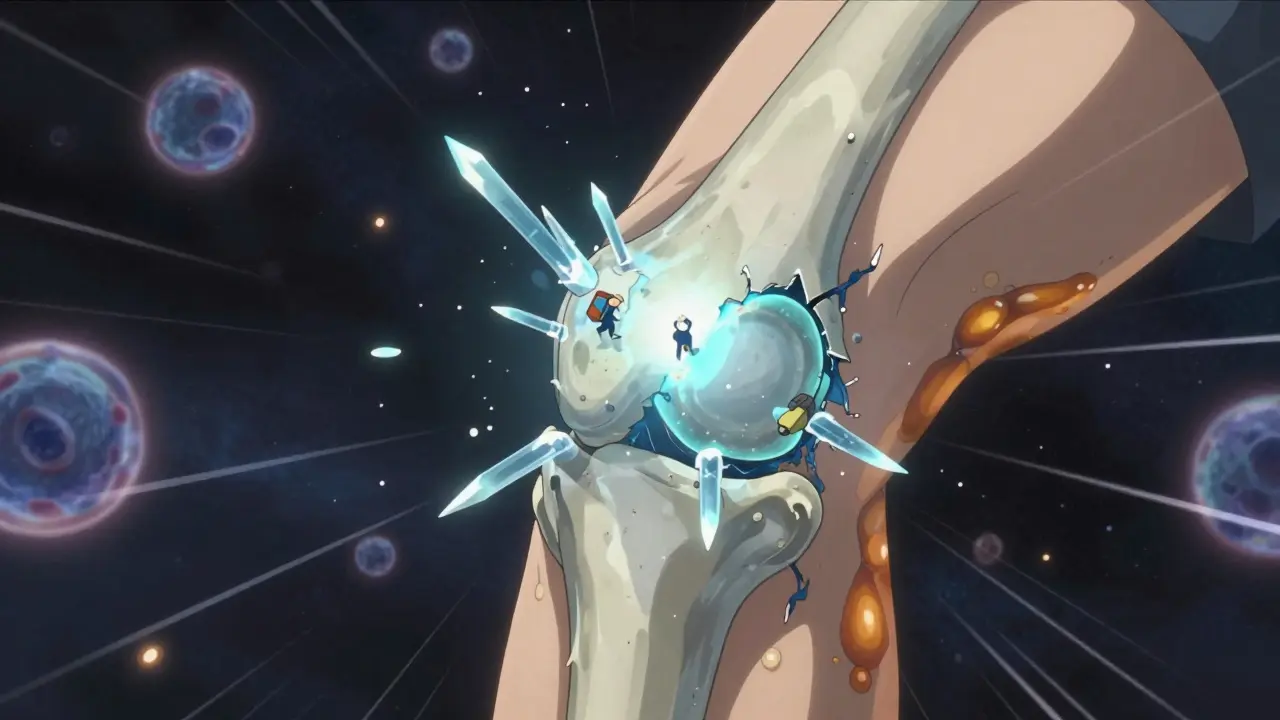
Osteoarthritis starts quietly. The smooth, slippery cartilage that cushions your joints-like the ones in your knees, hips, and hands-begins to fray. Under a microscope, you’d see tiny cracks forming on the surface, then deeper erosion. Chondrocytes, the cells that maintain cartilage, go into overdrive trying to repair the damage, but they can’t keep up. The collagen matrix that gives cartilage its strength starts to unravel.
This isn’t just about cartilage. The whole joint gets involved. Bone thickens around the edges, forming bony spurs called osteophytes. The synovial fluid that lubricates the joint thins out. Ligaments stretch and weaken. Even the fat pad around the knee can become inflamed. That’s why OA is now called a "whole joint disease," not just cartilage wear.
Unlike rheumatoid arthritis, which is autoimmune, OA isn’t your immune system attacking your joints. It’s mechanical stress meeting biological failure. Repetitive motion, past injuries, or excess weight overload the joint. The body tries to fix it, but the repair process goes wrong. Inflammation becomes chronic. Pain doesn’t come from the cartilage itself-there are no nerves there-but from the tissues surrounding it: bone, ligaments, and the joint lining.
Where Does OA Usually Show Up?
Not all joints are equally at risk. The most common sites follow a pattern:
- Knees: Affects 60% of people with OA. Weight-bearing and constant movement make them vulnerable.
- Hips: Seen in 30% of cases. Pain often radiates to the groin or thigh.
- Hands: Especially the base of the thumb, ends of fingers, and middle finger joints. Bony bumps called Heberden’s and Bouchard’s nodes are common.
- Spine: Affects 20%, especially the neck and lower back. Can cause stiffness and nerve pressure.
OA doesn’t always hit both sides evenly. You might have worse pain in your right knee than your left. That’s a clue it’s not systemic-it’s mechanical. X-rays use the Kellgren-Lawrence scale to grade severity from 0 (no signs) to 4 (bone grinding on bone, major joint space loss).
How Is OA Different From Other Arthritis?
Confusing OA with other types of arthritis is common-and dangerous. Here’s how to tell them apart:
- OA vs. Rheumatoid Arthritis (RA): OA pain gets worse with activity and improves with rest. RA pain is often worse in the morning, lasts over an hour, and improves with movement. RA also causes swelling, fatigue, and affects organs. OA doesn’t.
- OA vs. Gout: Gout hits suddenly-intense pain, redness, heat, often in the big toe. It’s caused by uric acid crystals. OA creeps in slowly over months or years.
- OA vs. Post-Traumatic Arthritis: This is OA that follows a joint injury-a torn ACL, a broken bone. It can show up years later, even if the injury seemed to heal.
Knowing the difference matters because treatments vary. RA needs immune suppressants. Gout needs uric acid control. OA? It’s about reducing load, strengthening support, and managing pain without side effects.
Why Does Pain Get Worse Over Time?
Early OA feels like stiffness after sitting, or a dull ache after walking. But as it progresses, the pain becomes constant. Why?
As cartilage wears away, bones start to rub. The joint’s natural shock absorber is gone. The body responds by thickening bone, forming spurs, and tightening ligaments. Nerves in the joint capsule become hypersensitive. Inflammation doesn’t go away-it lingers. Muscle weakness around the joint makes things worse. You start avoiding movement, which leads to more stiffness, more pain, and a downward spiral.
And here’s the hidden trap: avoiding movement because of pain makes you more likely to gain weight, develop heart disease, or get diabetes. The WHO calls this a "vicious cycle." Less activity → more weight → more joint stress → more pain → even less activity.
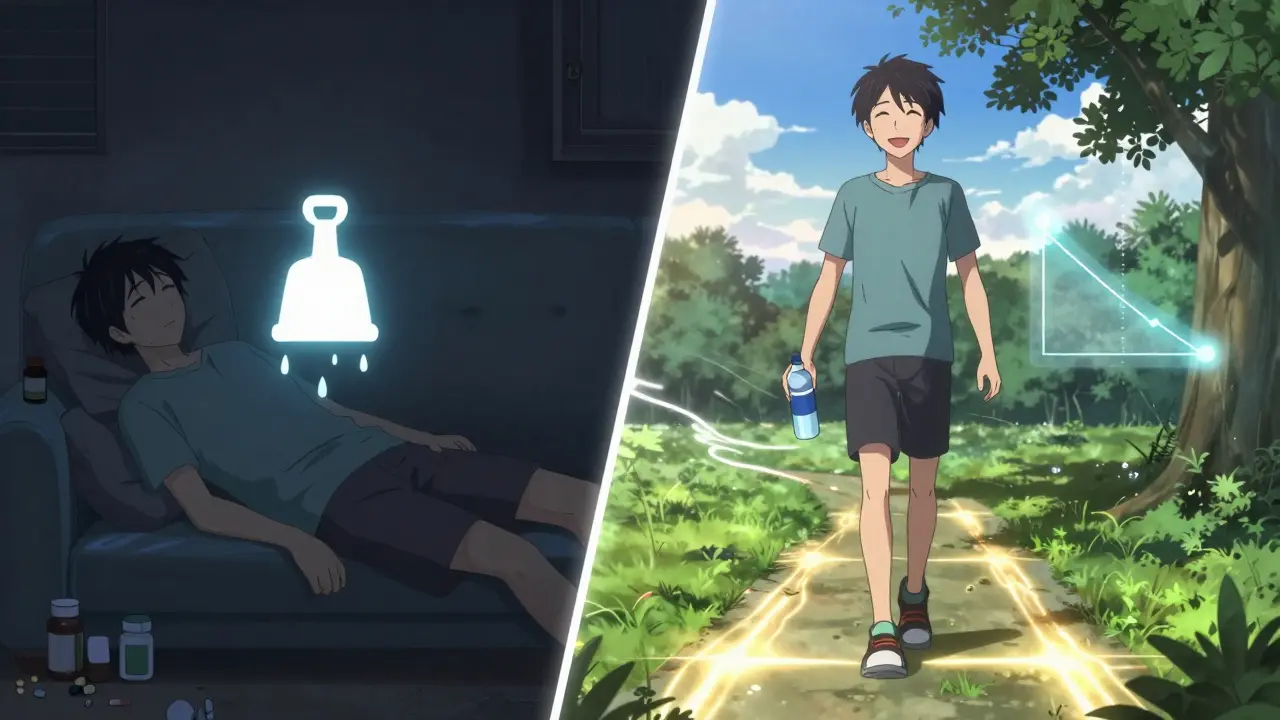
What Actually Works for Managing Pain?
There’s no cure for OA-but you can slow it down and feel better. The most effective strategies aren’t pills. They’re lifestyle changes backed by solid evidence.
1. Move-But Move Smart
Physical activity is the #1 treatment. Not just walking. You need strength, flexibility, and endurance. The Arthritis Foundation recommends:
- 3 times a week: 45 minutes of land-based exercise (walking, cycling, water aerobics)
- Strength training: Focus on muscles around the affected joint (quads for knees, glutes for hips)
- Stretching: Daily, especially in the morning
Studies show 80% of people who stick with this for 12 weeks cut their pain by 40% or more. The key? Consistency. Only 45% of people keep it up past 6 months. That’s why working with a physical therapist for 6-8 sessions makes a huge difference. They teach you how to move without hurting your joint.
2. Lose Weight-Even a Little
Losing 10% of your body weight can reduce knee OA pain by 50%. That’s not a guess-it’s from multiple clinical trials. For every pound you lose, you take 4 pounds of pressure off your knees. You don’t need to be thin. Just lighter than you are now.
3. Learn Joint Protection
Use your strongest joints. Sit down to put on shoes. Use a cart to carry groceries. Avoid kneeling or squatting. A physical therapist can show you how to do daily tasks without stressing your joints.
4. Try Injections-When Needed
Corticosteroid injections into the knee can cut pain by 50% for 4-6 weeks. They’re not for long-term use, but great for flare-ups. Hyaluronic acid shots (lubrication injections) have mixed results-some people swear by them, others don’t notice much. The OARSI guidelines say corticosteroids are the only injection with strong evidence.
5. New Options Are Here
In June 2023, the FDA approved tanezumab, a nerve growth factor blocker. In trials, it reduced pain 35% more than NSAIDs. It’s for moderate-to-severe OA when other treatments fail. It’s not a first-line option, but it’s a breakthrough for those who’ve run out of choices.
What Doesn’t Work (and What to Avoid)
Not everything marketed as an OA solution actually helps.
- NSAIDs (ibuprofen, naproxen): They help short-term pain, but 32% of people stop taking them because of stomach issues, kidney strain, or high blood pressure. Don’t use them daily unless your doctor says so.
- Glucosamine and chondroitin: Large studies, including those by the NIH, show they don’t work better than placebo for most people. Skip the expensive bottles.
- Cruciate ligament braces: Unless you’ve had surgery, most braces don’t help OA. They can make muscles weaker over time.
- Bed rest: Resting for more than a day or two makes stiffness worse. Movement is medicine.
And avoid "miracle cures"-stem cell injections advertised online? There are 387 clinical trials underway, but no FDA-approved stem cell therapy for OA yet. Many clinics charge thousands for unproven treatments. Don’t fall for it.
Who’s Most at Risk?
OA isn’t random. Certain factors raise your risk:
- Age: 34% of people over 65 have OA. But it’s not inevitable-43% of people with OA are under 65.
- Weight: Obesity doubles your risk for knee OA. Fat tissue releases inflammatory chemicals that damage joints.
- Gender: Women are more likely to get OA, especially after 50. Knee and hand OA are more common in women; men get more severe hip OA.
- Occupation: Construction workers have a 37% higher risk. Dancers, plumbers, and professional musicians are also at higher risk due to repetitive stress.
- History of injury: A torn meniscus or ACL injury years ago? You’re 5-10 times more likely to develop OA in that joint.
And here’s the scary part: by 2040, 78 million Americans could have OA-mostly because of rising obesity and aging populations.
What’s on the Horizon?
Research is moving fast. Scientists are looking for blood biomarkers that can detect OA before symptoms start. Dr. Virginia Byers Kraus at Duke says current X-rays are too late-we need tests that catch changes at the molecular level.
The CDC’s "Active People, Healthy Nation" program is rolling out free, community-based exercise classes in all 50 states. Early results show people who join these programs reduce pain by 40% and improve daily function by 30%.
Dr. Marc Hochberg predicts we’ll have a simple blood test for OA within five years. That could change everything-imagine catching it at Grade 1, before pain even starts, and stopping it with targeted lifestyle changes.
Real People, Real Results
On Reddit, a user named "KneePainSince40" wrote: "My knee OA started with occasional stiffness. Then I couldn’t walk more than 10 minutes without pain. I tried painkillers-they made me sick. I started physical therapy and lost 18 pounds. Now I walk 3 miles every morning. I didn’t fix my knee. I fixed my life." That’s the truth. OA isn’t about fixing a broken joint. It’s about rebuilding your whole approach to movement, weight, and daily habits. The best treatment isn’t a pill. It’s a routine. A walk. A healthy meal. A stretch. A decision to move, even when it hurts.
Can osteoarthritis be reversed?
No, osteoarthritis cannot be reversed. Once cartilage is lost, it doesn’t regrow on its own. But its progression can be slowed significantly-sometimes stopped-for years. Weight loss, exercise, and joint protection can prevent further damage and improve function, even in advanced cases. The goal isn’t to restore cartilage, but to reduce pain and keep you moving.
Is walking good for osteoarthritis?
Yes, walking is one of the best exercises for OA. It’s low-impact, improves circulation, strengthens muscles around the joint, and helps with weight control. Start slow-10 minutes a day-and build up to 30 minutes most days. Use supportive shoes. If it hurts too much, try walking in water or on a flat treadmill. Pain during walking should be mild and go away quickly after stopping. Sharp or lasting pain means you need to adjust your pace or get guidance from a physical therapist.
When should I see a doctor for joint pain?
See a doctor if joint pain lasts more than two weeks, gets worse over time, wakes you up at night, or makes it hard to do daily tasks like climbing stairs, buttoning clothes, or standing up from a chair. Also see a doctor if you have swelling, redness, or heat in the joint-this could signal something other than OA, like gout or infection. Early diagnosis means you can start managing it before it limits your life.
Do I need an X-ray to diagnose osteoarthritis?
Not always. A doctor can often diagnose OA based on your symptoms, age, and physical exam. X-rays are used to confirm severity, especially if surgery is being considered. But remember-X-rays show bone changes, not early cartilage damage. You can have significant pain with mild X-ray findings, or mild pain with severe X-ray changes. Your symptoms matter more than the image.
Are there any supplements that actually help with OA?
The only supplement with consistent evidence is vitamin D-if you’re deficient. Some people report relief with turmeric or omega-3s, but studies are mixed. Glucosamine and chondroitin don’t work better than a placebo for most people, according to large NIH trials. Avoid expensive joint supplements unless your doctor recommends them. Focus on food: fatty fish, leafy greens, berries, and nuts provide natural anti-inflammatory benefits.
Can I still exercise if I have severe OA?
Yes-but you need to choose wisely. High-impact activities like running or jumping should be avoided. But strength training, swimming, cycling, tai chi, and water aerobics are excellent. Even with severe OA, maintaining muscle around the joint reduces pressure on bone and cartilage. A physical therapist can design a safe program for you. Staying active is the best way to avoid losing mobility. Inactivity leads to more pain, not less.
If you’ve been told your joint pain is just part of aging, don’t believe it. OA is manageable. It’s not a death sentence for your mobility. With the right tools-movement, weight control, smart habits-you can keep living the life you love. Start today. One walk. One healthy meal. One stretch. That’s how it begins.
Kathryn Featherstone
December 18, 2025 AT 22:00I started physical therapy last year after my knee started giving out during walks. I was skeptical-thought it was just "old age." But after 8 weeks? I can carry groceries without wincing. No magic pills. Just consistent movement and learning how to move smarter. It’s not glamorous, but it works.
Also, losing 12 pounds didn’t "fix" my joint, but it took the pressure off enough that I sleep through the night now. Small changes, huge difference.
Nicole Rutherford
December 19, 2025 AT 23:28Ugh. Everyone says "just move more" like it’s that easy. Have you tried walking when your knee feels like ground glass? And don’t get me started on weight loss-like I haven’t tried every diet under the sun. You sound like one of those people who thinks pain is a motivational tool.
Also, glucosamine doesn’t work? Then why do half the pharmacies sell it like it’s holy water?
Mark Able
December 20, 2025 AT 05:00Hey I just read this and had to jump in-I’ve got OA in both hips and I’ve been doing water aerobics 5x a week for 2 years now. You think it’s hard? It is. But I used to need a cane. Now I hike. No joke.
Also, I got a standing desk and I swear it helped my lower back. Try it. Even if you hate it at first. Just try.
Dorine Anthony
December 20, 2025 AT 22:57My grandma had OA for 20 years. She never took a pill. Just walked every morning, ate fish twice a week, and never sat for more than an hour without standing up. She died at 92 with full mobility. No surgery. No injections. Just consistency.
Maybe the real cure isn’t new drugs-it’s old habits.
Marsha Jentzsch
December 22, 2025 AT 10:19Okay but who’s really behind this? The pharmaceutical companies? They don’t want you to know that movement works because then you won’t buy their $200/month creams and injections. And don’t even get me started on the FDA-they’re in bed with Big Pharma. Tanezumab? That’s just a fancy name for a controlled substance with a side of corporate greed.
Also, why are they pushing weight loss? Are you implying fat people are lazy? Because that’s ableist. And what about people who can’t lose weight due to meds or thyroid issues? Nobody talks about that. #OAisntyourfault
Janelle Moore
December 22, 2025 AT 19:06They say exercise helps but what if you can’t move? What if your body’s broken? What if you’ve been told to "just walk" for 10 years and it just made it worse? Who’s helping those of us who are stuck?
Also I heard from a guy on a forum that the government is putting fluoride in the water to make joints weaker so people will need more meds. I don’t know if it’s true but I’m scared now.
Henry Marcus
December 23, 2025 AT 19:57Let me tell you something no one’s saying: OA isn’t degeneration-it’s betrayal. Your body was built to last, but modern life? It’s a slow-motion assault. Processed food. Sitting all day. Shoes that turn your feet into plastic blocks. And now they want to inject you with nerve blockers like you’re some kind of broken robot?
Meanwhile, the real solution is walking barefoot on grass, eating real food, and sleeping like your ancestors did. But nope. We’re gonna keep selling pills and calling it progress.
William Liu
December 24, 2025 AT 21:43I was told I’d need a knee replacement by 50. I’m 53. Still walking. Still gardening. Still dancing with my grandkids. I didn’t do anything fancy. Just moved every day-even if it was just 10 minutes. And I stopped listening to people who said "you’re too old for that."
You’re not broken. You’re just out of practice. Start small. Be kind to yourself. It adds up.
jessica .
December 25, 2025 AT 00:07So they say lose weight but what about the people who live in food deserts? Who can’t afford fresh veggies? Who work two jobs and sleep 4 hours? This advice is for rich people with time to go to PT. Meanwhile, the system keeps ignoring the real problem: inequality.
And why is everyone so obsessed with walking? What about the people who can’t walk? Are they just supposed to give up?
Ryan van Leent
December 25, 2025 AT 03:37Glucosamine doesn't work? Whatever. I've been taking it for 5 years and I feel fine. Maybe it's placebo but if it helps me not scream when I get out of bed then who cares what some study says. Also I don't need a therapist to tell me how to walk. I've been walking since I was 2. This whole thing feels like overmedicated nonsense.
And why are we blaming fat people? My uncle was 300 lbs and never had OA. So maybe it's not about weight. Maybe it's about luck. Or genetics. Or something else they don't want you to know.