Corticosteroid Bone Health Risk Calculator
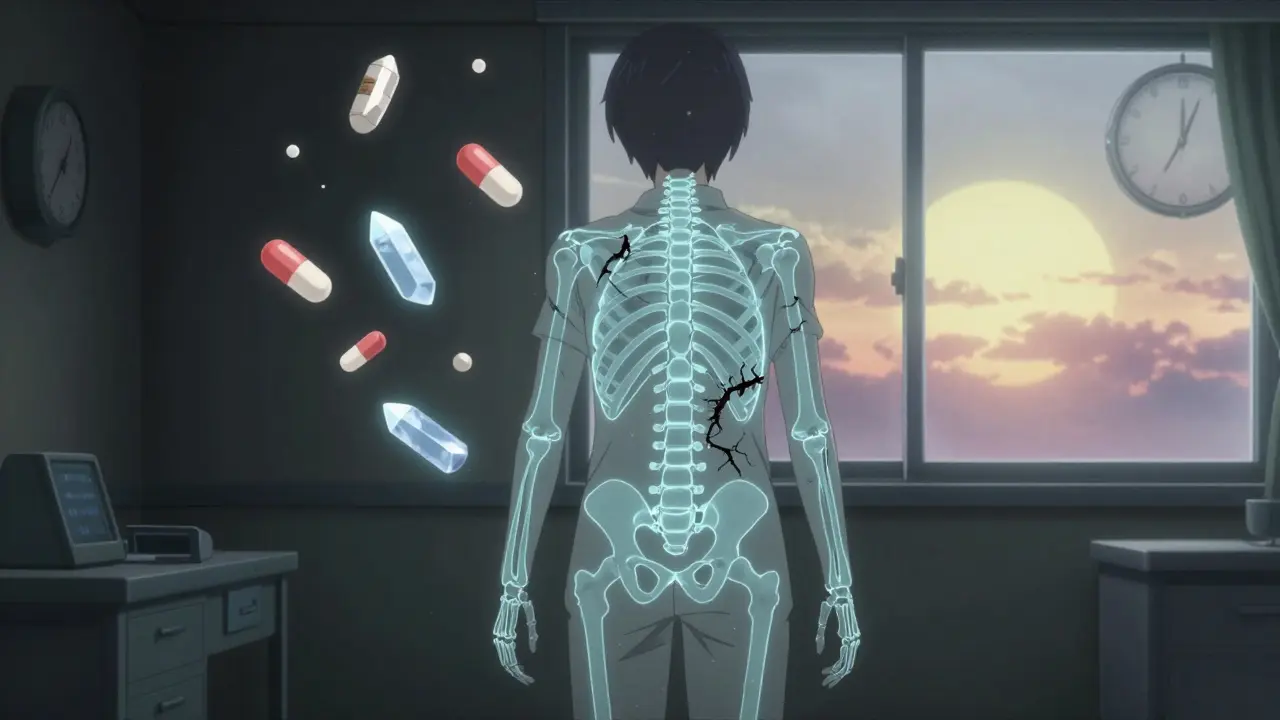
When you’re on long-term corticosteroids - whether for rheumatoid arthritis, lupus, asthma, or another chronic condition - you’re fighting one disease, but your bones are quietly losing ground. Corticosteroid-induced osteoporosis isn’t just a side effect; it’s a rapid, silent attack on your skeleton. Within the first three to six months of treatment, bone density can drop by 5% to 15%, and your risk of breaking a bone jumps by 70% to 100%. This isn’t something that happens years later. It starts fast, and if you don’t act early, you could end up with a fractured spine, hip, or wrist before you even realize your bones are weakening.
Why Corticosteroids Destroy Bone
It’s not just about getting older. Corticosteroids like prednisone don’t just suppress inflammation - they directly sabotage how your bones rebuild themselves. Your skeleton is always changing: old bone breaks down, new bone forms. Corticosteroids throw this balance out of whack. They shut down the cells that build bone (osteoblasts), make those cells die faster, and keep the cells that break bone (osteoclasts) alive longer. The result? Your bones lose density faster than they can recover.
On top of that, your body starts losing calcium. Corticosteroids reduce how much calcium your intestines absorb - by about 30%. They also make your kidneys flush out more calcium instead of holding onto it. Without enough calcium, your bones can’t stay strong. And because these drugs dull your bones’ response to movement, even walking or lifting weights becomes less effective at keeping them sturdy.
Each extra milligram of daily prednisone cuts your lumbar spine bone density by another 1.4% per year. At 7.5 mg or more per day, your fracture risk doubles. And here’s the scary part: half of all fractures linked to these drugs happen within the first year of treatment.
The First Line of Defense: Dose and Duration
The most powerful prevention tool isn’t a pill - it’s reducing the dose. If your doctor can lower your corticosteroid dose from over 7.5 mg to 7.5 mg or less per day, your fracture risk drops by 35% in just six months. That’s not a small win. It’s one of the biggest protections you can get.
But you can’t just stop your medication. You need to work with your doctor to find the lowest dose that still controls your condition. For some, that means switching to inhaled steroids for asthma or topical creams for skin conditions. For others, it means using steroid-sparing drugs like methotrexate or biologics to reduce reliance on prednisone altogether. The goal isn’t to eliminate steroids - it’s to use them as little as possible for as short a time as possible.
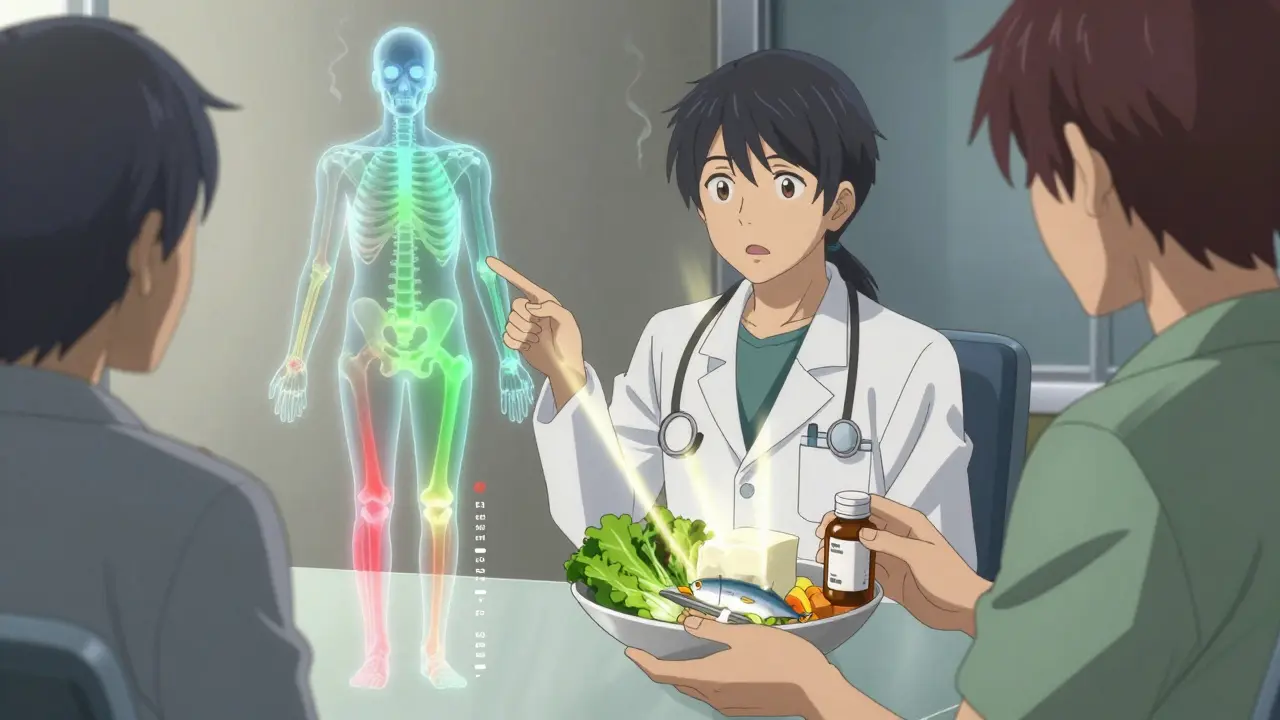
Calcium and Vitamin D: Non-Negotiable
If you’re on corticosteroids, you need calcium and vitamin D - not as an option, but as a baseline. The numbers are clear: you need 1,000 to 1,200 mg of calcium every day, mostly from food, with supplements filling the gap. That’s about three servings of dairy or fortified plant milk, plus leafy greens and canned fish with bones. Most people don’t get enough from diet alone.
Vitamin D is just as critical. You need 600 to 800 IU daily, but many experts recommend 800 to 1,000 IU to make sure your blood levels hit at least 20 ng/mL. Studies show that taking 1,000 mg calcium and 500 IU vitamin D together cuts bone loss in the spine by 0.72% per year. Without them, people on steroids lose about 2% per year. That’s a huge difference.
And here’s the catch: many people on steroids never get tested for vitamin D levels. If you’re not sure what your level is, ask for a blood test. Low vitamin D doesn’t just hurt bones - it makes your immune system less balanced, which can make your original condition harder to control.
Movement Matters - Even If It Feels Hard
Weight-bearing exercise isn’t optional. You need at least 30 minutes of it most days. That means walking, stair climbing, dancing, or even gardening. These activities tell your bones to stay strong. But corticosteroids blunt that signal. Studies show your bones respond 25% less to movement than someone not on steroids.
Still, don’t give up. Even with reduced response, movement helps. It improves balance, reduces fall risk, and keeps muscles strong enough to protect your bones. If you’re in pain or have limited mobility, talk to a physical therapist. They can design a safe routine that works for your body. Resistance training with light weights or bands is especially helpful - it doesn’t need to be intense to be effective.
And quit smoking. Smoking alone increases fracture risk by 25% to 30%. If you’re on steroids and smoke, you’re stacking two major risks on top of each other. Cutting out alcohol helps too - limit it to under three units a day. Heavy drinking weakens bones further and increases fall risk.
When Medication Becomes Necessary
If you’ve been on steroids for three months or more and you’re over 50, or if you’ve had a fracture before, you’re in the high-risk group. That’s when medication kicks in.
The first-line drug for most people is a bisphosphonate. Risedronate (5 mg daily or 35 mg weekly) cuts vertebral fractures by 70% and other fractures by 41%. Alendronate works too. These drugs slow bone breakdown and have been studied for over 20 years in steroid users.
If bisphosphonates don’t work for you - maybe because of stomach issues - there are other options. Zoledronic acid is a yearly IV infusion that boosts spine bone density by 4.5% in just 12 months. Denosumab is a six-month injection that increases spine density by 7%. And if your bones are already very weak (T-score below -2.5) or you’ve had multiple fractures, teriparatide is the strongest choice. It’s a daily injection that builds new bone, not just slows loss. In direct comparisons, it increases spine density 2.3 times more than alendronate.
But here’s the reality: only 15% of people on long-term steroids get the right treatment. Why? Because many doctors don’t know the guidelines. Many patients think bone loss is inevitable. And many don’t get tested.

The Hidden Gap: Who Gets Left Behind
Women are far more likely to get screened and treated than men. Studies show 76% of women receive some form of prevention - only 44% of men do. That’s not because men are less at risk. It’s because the problem is overlooked. Men on steroids are just as likely to fracture - but they’re less likely to be warned.
Only 31% of patients on long-term steroids get a bone density scan (DXA). Only 40% have calcium documented. Only 37% have vitamin D noted. And yet, every major guideline says these are mandatory steps.
The problem isn’t lack of knowledge - it’s lack of systems. In clinics where doctors get automatic alerts when a patient is prescribed more than 2.5 mg of prednisone daily, and where order sets include bone health checks, intervention rates jump from 40% to 92%. That’s not magic. It’s structure.
What You Can Do Right Now
- Ask your doctor: "Is my steroid dose the lowest possible?"
- Get a bone density scan if you’ve been on steroids for three months or more.
- Take 1,000-1,200 mg calcium and 800-1,000 IU vitamin D daily - no exceptions.
- Walk at least 30 minutes most days. Add light weights twice a week.
- Quit smoking. Limit alcohol.
- If you’ve had a fracture or have a T-score below -2, ask about bisphosphonates or teriparatide.
- Bring up bone health at every appointment. Don’t wait for your doctor to mention it.
There’s a myth that steroid-induced bone loss is unavoidable. It’s not. The science is clear. The tools exist. The biggest barrier isn’t medicine - it’s awareness. You have more power than you think. Start today.
Can I prevent osteoporosis if I’ve been on steroids for years?
Yes - even if you’ve been on steroids for years, you can still improve bone strength. Bone density can increase by 3% to 8% within a year of starting proper treatment, including calcium, vitamin D, exercise, and medication like bisphosphonates. The earlier you start, the better, but it’s never too late to act.
Do I need a bone scan if I feel fine?
Absolutely. Osteoporosis has no symptoms until you break a bone. By the time you feel pain, damage is often severe. A DXA scan is painless, takes less than 15 minutes, and is the only way to know your true bone density. Guidelines recommend one at the start of long-term steroid therapy and every 1-2 years after.
Are bisphosphonates safe for long-term use with steroids?
Yes. Bisphosphonates like risedronate and alendronate have been used safely in steroid users for over 20 years. The most common side effect is mild stomach upset, which often improves with taking the pill correctly (on an empty stomach, with water, staying upright for 30 minutes). Serious side effects like jaw bone problems or atypical thigh fractures are extremely rare - far less common than the risk of breaking a hip or spine.
Why is vitamin D more important for steroid users?
Corticosteroids reduce how your body absorbs and uses vitamin D. Even if you get sunlight or eat fortified foods, your levels may still be low. Low vitamin D means your body can’t use calcium properly, and your bones weaken faster. That’s why higher doses (800-1,000 IU) are recommended - to overcome this interference.
Can I stop taking steroids if my bones are weak?
No - stopping steroids suddenly can be life-threatening. If your condition requires them, you must taper under medical supervision. The goal is not to stop, but to reduce the dose as much as possible while keeping your primary disease under control. Bone protection should happen alongside your ongoing treatment.