When you take more than one medication, your body doesn’t treat them like separate guests at a party. It tries to process them all at once-and sometimes, they get in each other’s way. This is called a pharmacokinetic drug interaction. It’s not about how the drugs make you feel together; it’s about how one drug changes how your body handles another. These changes can make a drug too strong, too weak, or even dangerous. And while doctors and pharmacists work hard to catch these problems, you’re the most important person in the room when it comes to staying safe.
How Your Body Moves Drugs Around
Your body has a four-step system for handling drugs: absorb, distribute, metabolize, and excrete. Think of it like a delivery route. First, the drug gets absorbed into your bloodstream-usually through your stomach or intestines. Then it’s carried around by your blood. Next, your liver breaks it down. Finally, your kidneys flush it out. Any step in this chain can be disrupted by another drug, food, or supplement.Let’s say you take a painkiller and an antacid at the same time. The antacid makes your stomach less acidic. That’s fine for heartburn, but if you’re also taking ketoconazole (an antifungal), it won’t absorb properly. The result? The antifungal doesn’t work. You might keep getting infections because the drug never reached the right level in your blood.
When Food Gets in the Way
Some foods don’t just change how your meal tastes-they change how your medicine works. Grapefruit juice is the most famous example. It doesn’t just affect one drug. It interferes with over 85 prescription medications, including some statins for cholesterol, blood pressure pills, and anti-anxiety drugs. The juice blocks an enzyme in your gut called CYP3A4, which normally helps break down these drugs. Without it, too much of the drug enters your bloodstream. That can lead to dizziness, muscle damage, or even heart rhythm problems.Another common problem? Dairy and antibiotics. If you take tetracycline or doxycycline with milk, yogurt, or cheese, the calcium binds to the antibiotic and stops it from being absorbed. Up to half the dose can be wasted. The fix? Wait at least two to three hours between your antibiotic and any dairy product.
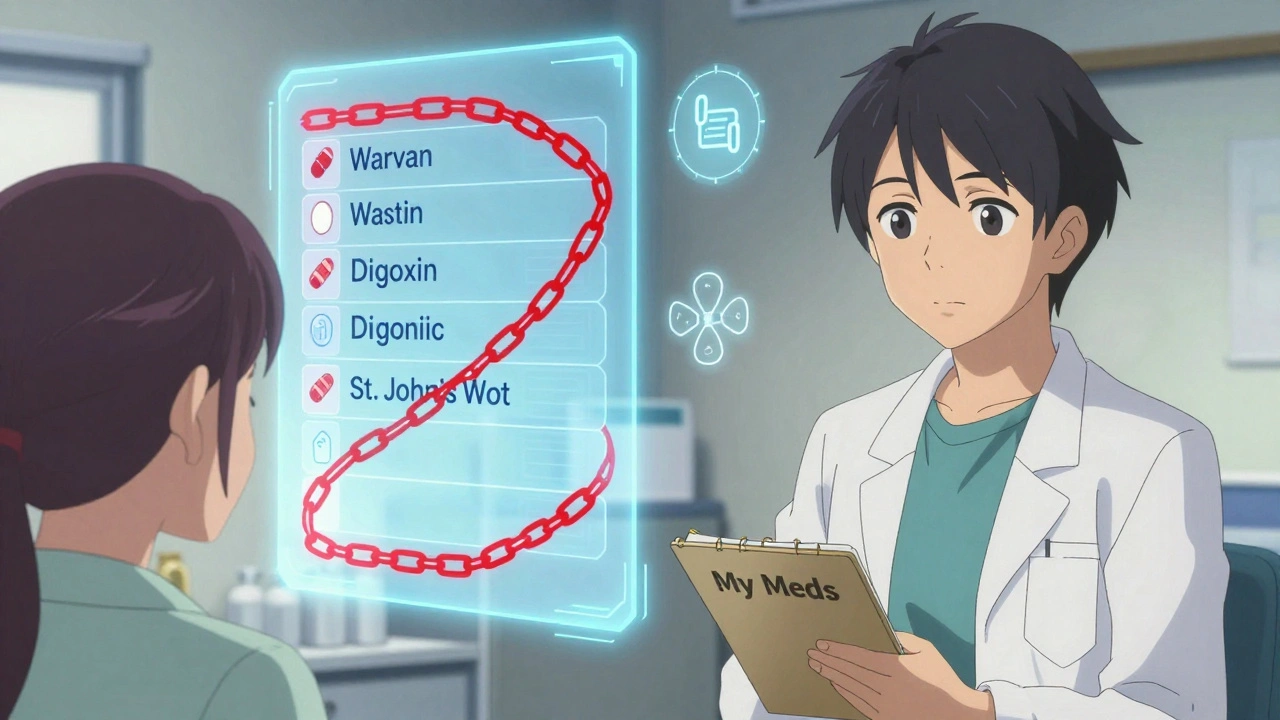
What Happens When Drugs Fight Over Space in Your Blood
Once a drug gets into your blood, it doesn’t float around freely. Most of it sticks to proteins like albumin, like a taxi holding onto a passenger. Only the unattached (free) part can do its job. But sometimes, two drugs want the same ride. Warfarin, a blood thinner, is one of the most sensitive to this. If you take diclofenac (a painkiller) at the same time, it can push warfarin off the protein, leaving more free warfarin in your blood. That can increase your risk of serious bleeding.But here’s the thing: this kind of interaction doesn’t always cause trouble. Your body usually adjusts by breaking down the extra free drug faster. That’s why it’s only a real concern with drugs that have a very narrow safety window-like warfarin, digoxin, or phenytoin. If you’re on one of these, your doctor will monitor your levels closely.
The Liver’s Hidden Battle: Metabolism Interactions
Most serious drug interactions happen in your liver. That’s where enzymes-especially the CYP450 family-break down drugs. Think of them as tiny scissors cutting up medicine so your body can get rid of it. Sometimes, one drug cuts those scissors short (inhibition). Other times, it makes more scissors (induction).Take metoprolol, a heart medication. If you also take propafenone (another heart drug), propafenone blocks the enzyme that breaks down metoprolol. That means metoprolol builds up. Too much can slow your heart too much, causing dizziness or fainting. Doctors will lower your metoprolol dose if you start taking propafenone.
On the flip side, St. John’s Wort-a popular herbal supplement for mood-tricks your liver into making more enzymes. If you’re on birth control, this can make it less effective. If you’re on an antidepressant like sertraline, it can drop the levels so low that your symptoms come back. Even more dangerous: St. John’s Wort can interfere with HIV meds, transplant drugs, and some cancer treatments.
Another big one: clarithromycin (an antibiotic) and midazolam (a sedative). Together, they can make you dangerously sleepy. This isn’t theoretical. Emergency rooms see cases where people passed out after mixing these two.

Your Kidneys Aren’t Just Filters
Your kidneys don’t just flush out waste-they’re selective. Some drugs use the same exit ramps. Probenecid, used for gout, blocks the kidney’s ability to clear cephalosporin antibiotics. That means the antibiotic stays in your system longer. That might sound good, but it can lead to kidney damage or allergic reactions.NSAIDs like ibuprofen or naproxen can do the same thing to methotrexate, a drug used for arthritis and some cancers. When they’re taken together, methotrexate levels can spike. That can cause severe bone marrow suppression, leading to infections or bleeding.
Then there’s digoxin, a heart medication with a very small safety margin. It’s pushed out of kidney cells by a protein called P-glycoprotein. If you take it with itraconazole (an antifungal), that protein gets blocked. Digoxin builds up. Too much can cause irregular heartbeat, nausea, or even death. This is why your doctor checks your digoxin levels regularly if you’re on other meds.
Real Risks, Real Cases
These aren’t just textbook examples. In 2022, a woman in her 80s was admitted to hospital after taking venlafaxine (an antidepressant) and propafenone (a heart rhythm drug). Both are processed by the same liver enzyme and both block the same transporter. Her venlafaxine levels jumped. She started seeing things that weren’t there-hallucinations-and became agitated. It took days to stabilize her.Another case: an elderly man on warfarin started taking a new painkiller. He didn’t tell his doctor. Two weeks later, he ended up in the ER with internal bleeding. His INR-a test that measures blood thinning-was dangerously high. He didn’t know the two drugs could interact. He didn’t know to ask.
According to the Institute for Safe Medication Practices, warfarin, insulin, and digoxin are the top three drugs involved in serious interaction-related emergencies. Together, they account for one-third of all interaction-related ER visits.
How to Protect Yourself
You don’t need to be a scientist to avoid dangerous interactions. Here’s what actually works:- Keep a full list of everything you take: prescriptions, over-the-counter pills, vitamins, herbs, and even CBD. Include the dose and how often you take it.
- Use one pharmacy for all your prescriptions. Pharmacists run checks you won’t even know about. In the U.S., this prevents about 150,000 bad reactions every year.
- Ask your doctor or pharmacist: “Could this interact with any of my other medicines?” and “Are there foods or drinks I should avoid?” Studies show asking these questions catches 63% more potential problems.
- If you’re on thyroid medicine, wait at least four hours after taking it before eating calcium-rich foods or taking antacids. That’s how long it takes for absorption to settle.
- Avoid grapefruit juice if you’re on any heart, blood pressure, or cholesterol medication. Check the label or ask your pharmacist.
- Don’t start herbal supplements without checking. St. John’s Wort, kava, and echinacea are common culprits.
What Your Doctor and Pharmacist Are Doing
Your healthcare team isn’t sitting idle. Electronic health records now flag about 85% of major drug interactions. But here’s the catch: doctors get so many alerts that they ignore nearly half of them. That’s why your role matters so much.Pharmacists do medication reviews that cut adverse events by 22% in older adults. They’re trained to spot the hidden risks-like a new antibiotic clashing with your blood thinner or a supplement interfering with your heart drug. If you’re on multiple meds, ask for a medication review. It’s free in many places, including the NHS in the UK.
Tools like Lexicomp and Micromedex help pharmacists and doctors make quick, evidence-based decisions. These aren’t just databases-they’re updated daily with new findings.
What’s Changing Now
Science is catching up fast. In 2023, researchers found 12 new interactions involving diabetes drugs and kidney transporters. The FDA now requires drug makers to test for CYP enzyme effects before approval. And more than 340 drug labels now include genetic information-like whether you’re a slow or fast metabolizer of certain drugs.Genetic testing for drug response is becoming more common. If you’re a poor metabolizer of CYP2C19, you might need a different blood thinner than someone who breaks it down quickly. This isn’t sci-fi-it’s already in use in some hospitals.
Telehealth platforms now include interaction checkers. If you’re seeing your doctor online, they can run a quick scan of your meds before the appointment. In the U.S., 78% of major health systems have added this by 2023.

Nnaemeka Kingsley
December 1, 2025 AT 20:06Man this is wild. I took that antibiotic with yogurt once and it did nothing. Thought I was crazy till I read this. Now I wait 3 hours like a boss.
Kshitij Shah
December 1, 2025 AT 21:13So grapefruit juice is basically a drug cheat code? Cool. I guess that’s why my uncle ended up in the ER. He thought it was ‘healthy’ and kept drinking it with his statin. RIP his liver.
Walker Alvey
December 2, 2025 AT 21:34People die because they don’t read labels. Duh. This isn’t rocket science. Stop being lazy and take responsibility for your own body. Your pharmacist isn’t your babysitter.
Michelle Smyth
December 3, 2025 AT 12:12Interesting how the author anthropomorphizes the liver as if it’s a bouncer at a club. CYP450 enzymes aren’t ‘scissors’-they’re cytochrome P450 isoforms with substrate-specific catalytic activity. This post is dangerously reductive.
patrick sui
December 5, 2025 AT 00:00So if I’m on warfarin and take ibuprofen… it’s not just stomach irritation? It’s pushing warfarin off albumin like a drunk guy kicking someone off a couch? 😅 I’ve been taking Advil for migraines for years… time to talk to my doc. Thanks for the wake-up call.
Declan Flynn Fitness
December 5, 2025 AT 14:11Biggest thing I tell my clients: one pharmacy. Always. I had a guy on 12 meds from 5 different places. One of them gave him a statin + grapefruit juice combo. He almost lost a leg. Don’t be that guy.
Adrian Barnes
December 6, 2025 AT 03:24It is an ethical failure of modern medicine that patients are expected to be pharmacologists. The burden of safety should not rest on the untrained. This post, while informative, is a symptom of a broken system where profit outweighs prevention.
Irving Steinberg
December 7, 2025 AT 11:14St. John’s Wort is basically the weed of the pharmaceutical world. 🌿 It’s everywhere and nobody talks about it. I took it for ‘mood’ and my birth control failed. Now I have a kid I didn’t plan. Thanks, nature.
Patrick Smyth
December 8, 2025 AT 12:05I’ve been taking metoprolol for 7 years and just started propafenone last month. I’ve been dizzy since day 3. Is this it? Am I going to pass out? Should I go to the hospital? I’m scared. Someone help.
ANN JACOBS
December 9, 2025 AT 15:48As someone who has spent over two decades in clinical pharmacy, I can tell you that the most profound change in patient safety has been the integration of real-time interaction-checking algorithms into electronic prescribing systems. When these tools are properly calibrated and not overridden by alert fatigue, they reduce preventable adverse drug events by as much as 41% in high-risk populations-particularly the elderly, polypharmacy patients, and those with renal impairment. This is not anecdotal; it is evidence-based, and it is scalable.
Kay Lam
December 11, 2025 AT 13:44My grandma took digoxin and itraconazole together and ended up in the ICU. She didn’t know the antifungal was the problem. The doctors said her levels were off the charts. She’s fine now but we all learned the hard way. I made a chart for her: meds, times, foods to avoid. Now she carries it in her purse. Simple things save lives.
Declan O Reilly
December 11, 2025 AT 21:42It’s funny how we treat our bodies like cars with manuals we never read. You wouldn’t throw random oil into your engine without checking the manual. But we dump pills into our systems like confetti at a parade. Maybe the real problem isn’t the drugs-it’s the attitude. We think we’re invincible till our liver screams.
Lydia Zhang
December 13, 2025 AT 10:19My doctor didn’t ask about my turmeric supplements. Now I know better.