When a pharmacist swaps a brand-name drug for a generic, they’re not just saving money-they’re stepping into a legal gray zone. In 2025, this isn’t just a routine pharmacy task. It’s a high-stakes decision with real consequences. A patient could suffer a seizure, go into thyroid crisis, or bleed uncontrollably-not because the drug is faulty, but because the system doesn’t protect them, or the pharmacist, from the fallout.
Why Generic Substitution Isn’t Just a Cost-Saving Move
Generic drugs make up 90% of all prescriptions filled in the U.S. They cost 85% less than brand-name versions. That’s $1.67 trillion saved since 2009. But behind those numbers is a broken liability chain. Federal law, thanks to the 2011 PLIVA v. Mensing Supreme Court ruling, says generic manufacturers can’t change their drug labels-even if new safety data emerges. The brand-name maker owns the original label, but the generic maker must copy it exactly. So if a patient has a bad reaction, they can’t sue the generic company. And they usually can’t sue the brand-name maker either, because they didn’t make the drug the patient took. That leaves the pharmacist in the middle. If a patient gets hurt after a generic substitution, who’s responsible? In 23 states, the answer is: the pharmacist could be. In 27 states, the law says pharmacists have the same liability as if they’d dispensed the brand-name drug. But that’s not always true in practice. Courts don’t always agree. And patients? Most don’t even know they were switched.The Hidden Danger: Narrow Therapeutic Index Drugs
Not all drugs are created equal. For medications like warfarin, levothyroxine, and antiepileptics, tiny differences in how the body absorbs the drug can mean the difference between control and crisis. These are called narrow therapeutic index (NTI) drugs. The FDA says generics must be 80-125% bioequivalent to the brand. That sounds precise-until you realize that’s a 45% range. For a blood thinner like warfarin, a 10% shift in absorption can send a patient to the ER with internal bleeding. A 2017 study in Epilepsy & Behavior found that 18.3% of patients had therapeutic failure after switching generic antiepileptics. That’s nearly 1 in 5. In one documented case, a patient suffered permanent brain damage after a generic substitution. The court dismissed the lawsuit-because federal law blocked any claim against the generic manufacturer. The pharmacist? They were never named in the suit. But they still lost sleep over it. Patients aren’t blind to this. On Reddit’s r/pharmacy, hundreds have shared stories: “I switched to generic levothyroxine and felt like I was dying.” “My seizures came back after the pharmacy changed my meds.” A 2021 survey by the Patient Advocacy Foundation found 41% of patients didn’t know they’d been switched until they felt worse. And in states without mandatory notification laws, pharmacists aren’t required to tell them.State Laws Are a Patchwork-And That’s a Problem
There’s no national standard. Each state sets its own rules. In California, pharmacists must notify patients in writing and get consent before substituting NTI drugs. In Connecticut? No such requirement. And in Connecticut, pharmacists have seen 27% more malpractice claims related to substitution than in states with strong protections. Here’s how it breaks down:- Duty to substitute: 27 states require substitution if the prescription allows it. 23 states leave it up to the pharmacist.
- Patient notification: Only 18 states require pharmacists to inform patients beyond the label.
- Right to refuse: 32 states let patients say no to a generic. 18 don’t.
- Liability protection: 27 states shield pharmacists from greater liability for generics. 23 don’t. In Massachusetts, a pharmacist was sued after a patient had a stroke following a generic switch. The court said the pharmacist had a duty to know the risks-and didn’t.
What Pharmacists Are Doing to Protect Themselves
Most pharmacists aren’t waiting for lawmakers to fix this. They’re taking matters into their own hands. The American Society of Health-System Pharmacists recommends a 7-step risk-reduction plan:- Know your state’s law. Check the National Association of Boards of Pharmacy’s annual compendium. Laws change. Don’t rely on memory.
- Use EHR alerts. Set up electronic flags for NTI drugs. If a prescription comes in for levothyroxine, the system should pop up: “NTI drug. Verify substitution protocol.”
- Get written consent. Use a simple form: “I understand this generic version may differ from my previous brand. I accept this substitution.” Have the patient sign it. File it.
- Call the prescriber. If you’re unsure, ask the doctor. Many physicians don’t realize how risky substitution can be for NTI drugs. A quick call can prevent a disaster.
- Track every substitution. Record the brand, generic, lot number, and date. If a problem arises, you need to trace it back.
- Do a liability risk assessment. Use the 27-point checklist from the Journal of the American Pharmacists Association. It covers everything from documentation to communication.
- Get extra insurance. Standard malpractice policies often exclude substitution-related claims. Buy supplemental coverage. It costs $300-$800 a year. Worth it.
Patients Want to Be Informed-And They’re Fighting Back
The National Association of Chain Drug Stores surveyed 452 pharmacists in 2022. 87% said they support mandatory patient notification. Why? Because patients are asking. They’re reading labels. They’re noticing changes in how they feel. And they’re calling out pharmacies that don’t tell them. A 2023 GoodRx review of 15,783 users showed 82% satisfaction with generics for common drugs like metformin and lisinopril. But for NTI drugs? Satisfaction drops to 51%. That’s not because generics are bad. It’s because patients feel blindsided. In one case, a patient in Florida sued her pharmacy after switching to a generic antiepileptic. She had a seizure and lost her job. The pharmacy had followed state law-no notification required. But the court awarded her damages anyway, citing “lack of informed consent.” The verdict wasn’t based on the law. It was based on fairness.
The Bigger Picture: Is the System Sustainable?
The Congressional Budget Office estimates the current liability gap will cost the healthcare system $4.2 billion annually by 2030 in untreated adverse events. The Institute for Clinical and Economic Review says fixing it could raise generic prices by 7-12%. But it would prevent 14,000 serious injuries every year. Some states are trying. In 2023, 11 states introduced the “Generic Drug Safety Act.” It would require brand-name manufacturers to update labels within 30 days of new safety data-and force generic makers to adopt those changes within 60 days. That’s a start. The FDA’s 2023 pilot program for label changes has approved 68% of requests-but only 12% came from generic companies. They’re still waiting for permission. The most promising solution? “Consensus labeling.” A single, standardized label for all versions of a drug-brand or generic-updated by a neutral body based on real-world data. It’s being piloted in five states under the Interstate Pharmacy Compact. If it works, it could end the legal chaos.What You Need to Do Today
You don’t need to wait for legislation. You don’t need to hope for federal action. You can act now.- Stop assuming substitution is low-risk. It’s not.
- Know your state’s law. Every year. Update your checklist.
- Use technology. Alerts, forms, logs-don’t rely on memory.
- When in doubt, call the prescriber. Or don’t substitute.
- Always tell the patient. Even if the law doesn’t require it.
- Get the right insurance. Don’t gamble with your license.
Can a pharmacist be sued for substituting a generic drug?
Yes, in 23 U.S. states, pharmacists can be held liable for harm caused by generic substitution if they fail to follow state laws-such as not notifying the patient or substituting an NTI drug without consent. Even in states with liability protections, courts have ruled against pharmacists when documentation or communication was lacking. Federal law shields generic manufacturers, but not pharmacists.
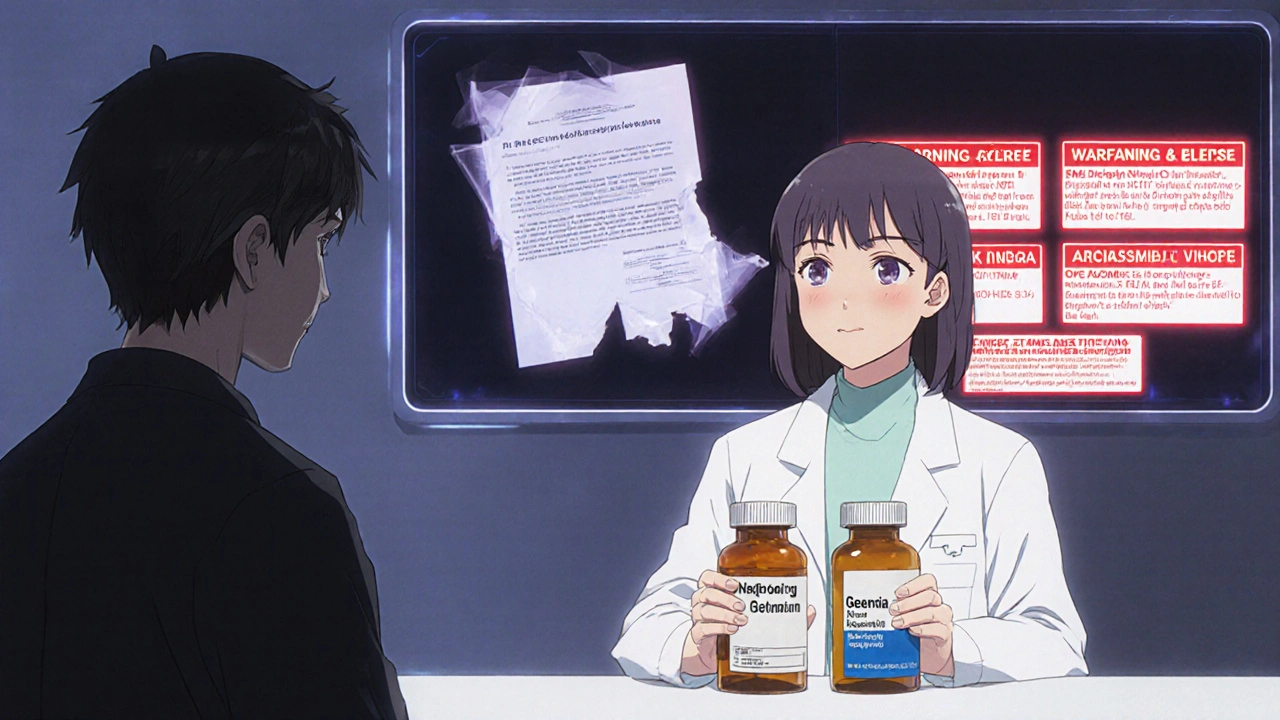
Which drugs are most dangerous to substitute?
Narrow therapeutic index (NTI) drugs are the highest risk. These include levothyroxine (for thyroid), warfarin (blood thinner), phenytoin and other antiepileptics, lithium, and cyclosporine. Small changes in blood levels can cause toxicity or therapeutic failure. Studies show 18-20% of patients on substituted NTI drugs experience adverse events.
Do I have to tell patients they’re getting a generic?
In 18 states, yes-by law. In the other 32, it’s optional. But even where it’s not required, best practice demands you inform patients. A 2021 survey found 41% of patients didn’t know they’d been switched until they had side effects. Clear communication reduces lawsuits and builds trust.
Can I refuse to substitute a generic drug?
Yes, in all 50 states and D.C., pharmacists can refuse substitution if they believe it’s unsafe-especially for NTI drugs. Many pharmacists do this routinely. In fact, 74% of pharmacists surveyed in 2022 admitted they’ve refused substitutions for high-risk drugs due to liability concerns, even when state law allowed it.
Is generic substitution legal for biologics?
Yes, but it’s new and complex. As of 2025, 45 states have laws allowing substitution of biosimilars (generic versions of biologic drugs like insulin or rheumatoid arthritis treatments). However, liability rules vary widely. Unlike small-molecule generics, biosimilars aren’t identical to the brand. Substitution without provider approval is still controversial, and many prescribers require “non-substitutable” labels.
What’s the best way to protect myself legally?
Follow the 7-step risk-reduction protocol: 1) Know your state’s laws, 2) Use EHR alerts for NTI drugs, 3) Get written patient consent, 4) Consult the prescriber when unsure, 5) Log all substitutions with batch numbers, 6) Complete annual liability assessments, and 7) Purchase supplemental malpractice insurance covering substitution. Document everything.
robert cardy solano
November 20, 2025 AT 16:05Man, I’ve seen this play out in my pharmacy. Patient comes in for levothyroxine, gets switched, calls back two weeks later saying they’re exhausted, gaining weight, feeling like crap. We didn’t even know they’d been switched until they told us. No one’s asking us to stop generics-just tell people when you swap ‘em. It’s not hard.
Rebecca Cosenza
November 21, 2025 AT 07:53This is why we need accountability. Not just ‘best practices’-real legal teeth. If you’re going to swap a drug that can kill someone, you damn well better get consent. No excuses. 🙄
Cinkoon Marketing
November 23, 2025 AT 01:48As someone who works in regulatory compliance in Canada, I can tell you-we don’t have this mess here. Generic substitution is allowed, but only if the prescriber doesn’t say ‘dispense as written.’ And we require pharmacists to document every swap and notify patients verbally AND in writing. No gray zones. No lawsuits. Just common sense. Why can’t the U.S. do this?
swatantra kumar
November 24, 2025 AT 23:15Bro, the FDA lets generics be 80-125% bioequivalent? 😂 That’s like saying two pizzas are the same if one is 20% smaller or 25% bigger. How is this legal? I’d rather pay extra and not end up in the ER. 🤦♂️
Pawan Jamwal
November 26, 2025 AT 12:50India makes 40% of the world’s generics and we don’t have this problem. Why? Because we don’t let greedy American corporations play games with patient safety. This is capitalism gone wild. Fix the system, not the blame.
Bill Camp
November 27, 2025 AT 01:45THEY’RE KILLING PEOPLE AND NO ONE’S BEING HELD ACCOUNTABLE?! THIS IS A MASSACRE. PHARMACISTS AREN’T DOCTORS-THEY’RE NOT SUPPOSED TO BE DECIDING WHO LIVES OR DIES BASED ON A STATE LAW THAT CHANGES EVERY YEAR. THIS IS A NATIONAL DISGRACE.
Lemmy Coco
November 27, 2025 AT 20:35i read this whole thing and i think the biggest problem is no one keeps good records. i work in a small pharmacy and we just started using ehr alerts for ntis and it changed everything. we had zero issues last month. also i typoed ‘levothyroxine’ 3 times while typing this lmao
rob lafata
November 28, 2025 AT 07:40Let me be the asshole here: pharmacists are getting sued because they’re lazy, overworked, and think ‘it’s just a generic’-like it’s a damn candy bar. You’re not just handing out pills, you’re playing Russian roulette with someone’s thyroid, brain, or heart. If you can’t handle the liability, go work at a gas station. This isn’t rocket science-it’s basic damn responsibility.
Matthew McCraney
November 29, 2025 AT 01:14They’re hiding this from us. Big Pharma and the FDA are in bed together. You think they want you to know that your generic blood thinner might be 30% less effective? Nah. They want you to stay quiet and keep paying for your meds. This is how they control you. Wake up. 🕵️♂️
serge jane
November 30, 2025 AT 19:49I’ve been a pharmacist for 27 years and I still don’t know if I’m doing the right thing. The law changes every year. The science keeps evolving. And patients? Most of them don’t even care until they’re shaking in the ER. Maybe the real question isn’t who’s liable-it’s whether we’ve built a system that expects humans to make perfect decisions under impossible conditions. We’re not machines. We’re just trying not to kill someone today.
Nick Naylor
November 30, 2025 AT 22:11Per 21 CFR 314.94, 21 U.S.C. §355(j), and state pharmacy board regulations (e.g., Cal. Bus. & Prof. Code §4052), substitution protocols are codified, yet inconsistent across jurisdictions-creating a liability fragmentation matrix that disproportionately impacts community-based practitioners who lack institutional risk management infrastructure. Mandatory EHR integration and federal preemption of state-level substitution statutes are the only viable path forward.