When a pharmacist hands you a different pill than what your doctor prescribed, it’s natural to wonder: Is this safe? Did they just swap one drug for another without telling anyone? You’re not alone in feeling uneasy. But here’s the truth most people don’t know: what’s happening isn’t random. It’s called therapeutic interchange, and it’s a carefully controlled process-but only within the same drug class. Contrary to what the title suggests, providers don’t switch you from, say, a blood pressure pill to a diabetes drug. That would be dangerous. Therapeutic interchange is about swapping one beta-blocker for another, or one SSRI for another-not crossing therapeutic lines.
What Therapeutic Interchange Actually Means
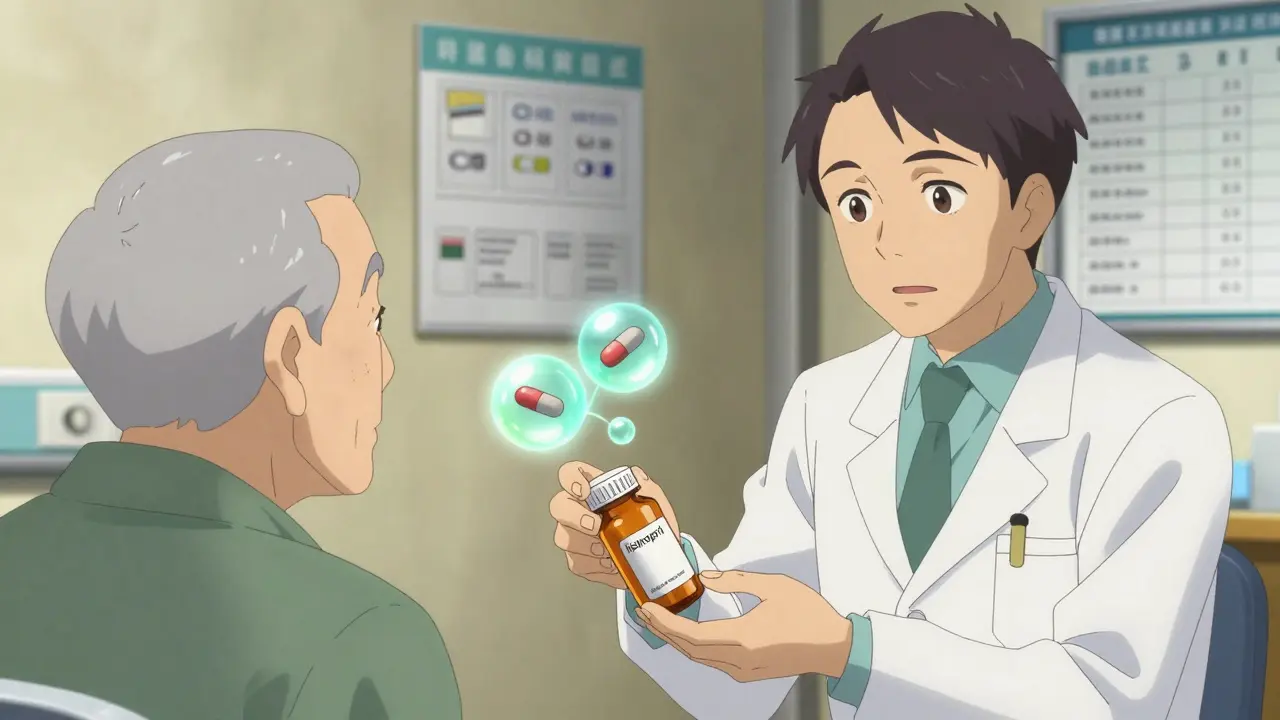
Therapeutic interchange is when a pharmacist substitutes a prescribed medication with a different drug from the same therapeutic class that’s expected to work just as well, but costs less. Think of it like switching from one brand of running shoe to another-same purpose, different design, similar performance. If your doctor prescribes lisinopril for high blood pressure, and your facility’s formulary prefers enalapril, a pharmacist might swap them. Both are ACE inhibitors. Both lower blood pressure. Both have similar side effect profiles. But enalapril might cost $12 a month instead of $45. This isn’t generic substitution. Generic substitution is swapping brand-name lisinopril for generic lisinopril-same chemical, same manufacturer, just cheaper. Therapeutic interchange is moving between different chemicals that do the same job. The American College of Clinical Pharmacy (ACCP) defines it clearly: it’s a substitution between drugs that are chemically different but therapeutically equivalent. That’s the rule. No exceptions. No jumping classes.Who Decides What Gets Swapped?
You might think a pharmacist makes this call on their own. They don’t. It’s not that simple. Every therapeutic interchange program is built on a formulary-a list of approved medications a hospital or long-term care facility has agreed to use. This list isn’t created by a single person. It’s developed by a Pharmacy and Therapeutics (P&T) Committee, made up of doctors, pharmacists, nurses, and sometimes even patients or their advocates. They review clinical data, cost, side effects, and real-world outcomes before approving any drug for inclusion. Once a drug is on the formulary, pharmacists can swap it in for another drug in the same class-but only if the original prescription matches the criteria in the formulary policy. For example, if the formulary says “enalapril is preferred over lisinopril for heart failure patients over 65,” then a pharmacist can make that switch without calling the doctor, as long as the patient fits that profile. But here’s the catch: not every state lets pharmacists do this automatically. In some places, the prescriber has to sign a Therapeutic Interchange (TI) letter upfront. That letter says, “I’m okay with switching from drug A to drug B for all my patients on this medication.” Once signed, the pharmacy can make the swap every time without asking again. In other states, the pharmacist must call the doctor for every single switch. That slows things down, creates more work, and sometimes delays care.
Why Hospitals Love It-And Why Community Pharmacies Struggle
Hospitals and skilled nursing facilities are the main users of therapeutic interchange. Why? Because they manage hundreds of patients on the same medications every day. When you’re paying $50,000 a month for heart medications alone, even a 30% savings adds up fast. SRX Technologies reports skilled nursing homes save tens of thousands of dollars monthly just by switching to formulary-preferred drugs. That money can go toward better staffing, better meals, or more therapy sessions. But in your local pharmacy? It rarely happens. Why? Because community pharmacists don’t have access to the same formularies. They don’t control the prescribing. And most prescribers don’t sign those TI letters for outpatient settings. If a community pharmacist wants to swap your atorvastatin for rosuvastatin, they have to call your doctor. Most doctors say no-not because they don’t trust the science, but because they don’t want to deal with the phone tag. A 2021 health policy analysis found that in outpatient settings, therapeutic interchange only happens when the prescriber has already agreed to it. Otherwise, it’s blocked by workflow, liability fears, and lack of communication systems.When It Works-and When It Goes Wrong
Therapeutic interchange works best when:- The drugs have proven clinical equivalence (same target, same outcomes)
- The formulary was built with input from multiple disciplines
- The patient has no history of adverse reactions to the substitute
- The change is documented and communicated to all caregivers
- A pharmacist swaps a sulfa-based antibiotic for a penicillin-based one-different classes, different risks
- A patient has a known sensitivity to one drug in the class and the substitute triggers the same reaction
- The prescriber wasn’t consulted, and the patient ends up with worse side effects
- The formulary is outdated or based on cost alone, not clinical data

What Patients Need to Know
If you get a different pill, ask: “Is this the same kind of medicine as what I was supposed to get?” Don’t assume it’s a mistake. It might be therapeutic interchange. Ask if the change was approved by your doctor. Ask if it’s on your facility’s formulary. You have a right to know. If you’re on a medication that’s been switched and you feel worse-fatigue, dizziness, rash, mood changes-call your doctor. Don’t wait. Even if the swap was “approved,” your body might respond differently. Not all patients react the same way to drugs in the same class. And if you’re in a long-term care facility? Ask your care team if they use therapeutic interchange. Ask to see the formulary. You’re not just a patient-you’re part of the decision.The Bottom Line
Therapeutic interchange isn’t about cutting corners. It’s about smart, evidence-based care. It’s how hospitals reduce costs without sacrificing outcomes. It’s how patients get the same results for less money. But it only works when it’s done right-within the same class, with clear protocols, and with patient safety as the top priority. The idea that providers switch between different drug classes? That’s a myth. That’s not therapeutic interchange. That’s a dangerous error. Real therapeutic interchange is precise, regulated, and backed by decades of clinical research. It’s not a loophole. It’s a system. If you’ve ever wondered why your medication changed, now you know: it wasn’t random. It was planned. And if done properly, it’s one of the quietest, most effective ways healthcare saves money-without hurting patients.Can a pharmacist switch my medication to a different class without my doctor’s permission?
No. Therapeutic interchange only applies to drugs within the same therapeutic class-like switching one beta-blocker for another. Switching between different classes (e.g., from a statin to a blood thinner) is not therapeutic interchange and is never allowed without explicit prescriber approval. Doing so would be a clinical error and could be illegal depending on state laws.
Why do some pharmacies switch my meds while others don’t?
It depends on where you are. Hospitals and nursing homes often have formal formularies and P&T committees that authorize therapeutic interchange. Community pharmacies usually don’t have those systems in place. In most cases, a community pharmacist must call your doctor to get permission before making any substitution-even within the same class-unless your doctor signed a Therapeutic Interchange (TI) letter ahead of time.
Is therapeutic interchange the same as using generics?
No. Generic substitution means replacing a brand-name drug with its exact chemical copy-like switching from Lipitor (atorvastatin brand) to generic atorvastatin. Therapeutic interchange is switching between two different drugs that do the same job-like switching from atorvastatin to rosuvastatin. Both are statins, but they’re chemically different. Generics are identical; interchange is different but equivalent.
What if I don’t want my medication switched?
You have the right to refuse. If a substitution is proposed, ask if it’s part of a formulary policy. If you’re uncomfortable, tell your pharmacist or doctor. Most formularies allow exceptions. You can request your original medication, and the pharmacy will honor it-though you may pay more out of pocket. Always speak up if you’ve had bad reactions to similar drugs in the past.
How do I know if my facility uses therapeutic interchange?
Ask your care team. In hospitals or long-term care facilities, formulary policies are often posted or available upon request. Look for signs like “Formulary Preferred” on your medication label or ask your pharmacist: “Is this change part of the facility’s therapeutic interchange program?” If they hesitate or can’t answer, it’s worth asking for clarification from your doctor.
Michael Burgess
January 4, 2026 AT 23:53Man, I got switched from lisinopril to enalapril last month and thought I was getting scammed. Turns out? Same class, same effect, saved me $30 a month. Pharmacist even printed me a little cheat sheet. Healthcare can be weird, but this? This is actually smart.
Also, why do people think pharmacists are just pill counters? They’re the unsung heroes keeping the system from collapsing.
Thanks for explaining this like I’m not a medical student.
Angela Goree
January 6, 2026 AT 02:12THIS IS WHY AMERICA IS FALLING APART. THEY’RE SWAPPING MEDS LIKE IT’S A GAME OF CARDS! NO ONE ASKED ME! I’M NOT A LAB RAT! MY DOCTOR NEVER SIGNED ANYTHING! THIS IS GOVERNMENT OVERREACH disguised as ‘cost-saving’!!
Neela Sharma
January 6, 2026 AT 21:59Here in India, we don’t have this system - but we do have generic swaps that feel like roulette. Still, I get it: if two drugs do the same thing and one costs 1/5th, why not? It’s not about the pill. It’s about the person behind it.
Just make sure the patient knows. Communication is the real medicine.
Tiffany Channell
January 7, 2026 AT 19:07Oh please. ‘Therapeutic interchange’ is just corporate speak for ‘we’re cutting corners so shareholders don’t cry.’ You think patients don’t notice when their mood swings after a ‘swap’? Or when they get a rash from a ‘chemically different but therapeutically equivalent’ drug? That’s not science. That’s greed wrapped in a white coat.
And don’t even get me started on ‘P&T Committees.’ Who’s on those? Pharma reps with expense accounts and a PowerPoint presentation.
Hank Pannell
January 8, 2026 AT 22:31Let’s unpack the epistemology here: if two drugs are ‘therapeutically equivalent,’ what does ‘equivalent’ even mean? Is it statistical non-inferiority in RCTs? Real-world outcomes in heterogeneous populations? Or just the lowest bid at the pharmacy benefit manager’s auction?
And if the formulary is developed by a committee, who gets excluded? The patient with rare metabolic quirks? The elderly with polypharmacy? The uninsured who can’t afford to ‘opt out’?
Therapeutic interchange isn’t a neutral act - it’s a value-laden decision masked as clinical efficiency. We need transparency, not just protocols.
Ian Detrick
January 9, 2026 AT 13:59People act like this is some secret conspiracy, but it’s just good economics. You want your meds to be affordable? This is how you make that happen without sacrificing outcomes. I’ve seen patients on $12/month meds live longer than those on $50 ones - because they actually take them.
Stop treating healthcare like a luxury brand. It’s a public good. And public goods need smart systems, not emotional reactions.
Haley Parizo
January 11, 2026 AT 12:34My grandma got switched from sertraline to fluoxetine after a ‘formulary update.’ She cried for three days. Said she felt like a different person. Turns out, the ‘equivalent’ drug had a different half-life and messed with her sleep cycle. She ended up in the ER.
‘Therapeutic interchange’ sounds nice until it’s your mom’s brain chemistry getting swapped like a coupon.
veronica guillen giles
January 12, 2026 AT 17:13Ohhh so THAT’S why my prescription changed without a peep? And I thought I was just bad at remembering what meds I was on.
Let me guess - the pharmacist didn’t call because they knew if they did, the doctor would say ‘no’ and then the hospital would lose money. Classic.
So… the system is designed to bypass the patient’s voice so the balance sheet stays pretty? Brilliant. Send me a medal for being a good little consumer.
Brittany Wallace
January 14, 2026 AT 01:04As someone who’s been on 7 different SSRIs in 5 years, I can say: not all ‘equivalent’ drugs feel equivalent. Some days, the difference is like switching from a sedan to a motorcycle - same destination, different ride.
But I also get why hospitals do it. My sister works in a nursing home - they’re drowning in paperwork and budgets. This system lets them breathe.
So maybe the answer isn’t to kill therapeutic interchange… but to give patients a real voice in it. Like, an opt-out button that doesn’t require a lawyer.
Angela Fisher
January 15, 2026 AT 22:06EVERYTHING IS A CONTROLLED EXPERIMENT. YOU THINK THIS IS JUST ABOUT COST? NO. THEY’RE TESTING HOW OUR BODIES RESPOND TO DRUG SWAPS TO SEE IF WE’LL BECOME MORE DEPENDENT ON THE SYSTEM. THEY’RE USING US AS LAB RATS. THE FORMULARY? IT’S CODED. THE P&T COMMITTEE? THEY’RE ALL IN ON IT. PHARMACEUTICAL COMPANIES OWN THE HOSPITALS, THE PHARMACISTS, THE DOCTORS - AND NOW THEY’RE SWITCHING OUR MEDS TO SEE HOW LONG IT TAKES FOR US TO JUST ACCEPT IT WITHOUT QUESTION.
THEY WANT US TO BECOME LIKE THE INMATES IN THE ASYLUM WHO STOP ASKING WHY THEY’RE LOCKED UP.
ASK YOUR PHARMACIST: WHO FUNDED THE LAST FORMULARY REVIEW? I DARE YOU.
Shanahan Crowell
January 17, 2026 AT 13:19Look - I get the fear. But if you’re going to get mad about this, get mad at the system that makes $45 pills necessary in the first place.
Therapeutic interchange isn’t the villain - it’s the workaround. The real villain is a market that lets one company charge 10x more for the same molecule just because they own the brand name.
Let’s fix the root problem, not the symptom. And yes - patients should be informed. But don’t throw out the baby with the bathwater.
Brittany Wallace
January 19, 2026 AT 01:00Actually, I just checked my last script - the pharmacist left a sticky note: ‘Formulary swap: rosuvastatin for atorvastatin. Doctor approved via TI letter.’
Turns out my doc DID sign one. I just never knew it existed.
So maybe the problem isn’t the system… it’s the lack of communication. We need a simple ‘Your med was swapped because X’ slip with every pickup. Not a novel. Just one line.