When doctors need to keep blood clots from forming after a heart attack or a stroke, they often turn to Ticlopidine is a second‑generation thienopyridine antiplatelet that blocks the P2Y12 receptor on platelets. Its close cousin, Clopidogrel is a third‑generation thienopyridine that also inhibits the P2Y12 receptor but with a different metabolic pathway. Both drugs are used to prevent platelet aggregation, yet they differ in potency, safety profile, cost and how the body processes them. If you’ve ever wondered which one is the "better" choice, this guide breaks down the science, the side‑effects, and the practical considerations you need to know in 2025.
How the Two Drugs Work - The Core Mechanism
Platelet aggregation starts when the P2Y12 receptor is activated by ADP (adenosine diphosphate). Blocking this receptor stops platelets from sticking together, reducing the risk of clots in arteries that supply the heart and brain. Both ticlopidine and clopidogrel are irreversible antagonists, meaning they bind covalently and the effect lasts for the lifespan of the platelet (about 7‑10 days).
The key distinction lies in how each drug is activated inside the body. Ticlopidine is metabolised mainly by the enzyme CYP2C19 into an active metabolite, while clopidogrel requires a two‑step activation that involves CYP2C19, CYP3A4 and CYP2B6. This extra step makes clopidogrel more sensitive to drug‑drug interactions, especially with strong CYP2C19 inhibitors like omeprazole.
Speed of Onset and Duration
- Ticlopidine: Takes about 3‑5 days to reach full antiplatelet effect. The half‑life of the active metabolite is roughly 12‑14 hours, so steady‑state is achieved after a week of dosing.
- Clopidogrel: Reaches near‑maximal inhibition within 4‑6 hours after a loading dose (300 mg) and 5‑7 days on a 75 mg maintenance dose. Its active metabolite has a half‑life of about 8 hours.
For patients who need rapid protection-such as after percutaneous coronary intervention (PCI)-clinicians often give a loading dose of clopidogrel. Ticlopidine lacks an approved loading regimen, which can be a drawback in urgent settings.
Effectiveness in Preventing Cardiovascular Events
Large clinical trials from the early 2000s, like the CURE and ISAR‑REACT studies, showed that clopidogrel reduces the combined endpoint of cardiovascular death, myocardial infarction (MI) and stroke by about 20 % compared with aspirin alone. Ticlopidine demonstrated similar efficacy in the CAPRIE trial, but its higher adverse‑event rate limited widespread adoption.
More recent real‑world data from the UK’s Clinical Practice Research Datalink (CPRD) in 2023 suggests that, after adjusting for baseline risk, clopidogrel still edges out ticlopidine in preventing recurrent MI (hazard ratio 0.85 vs 0.92).
Safety Profile - What Side‑Effects to Watch For
Both drugs raise the risk of bleeding, but the type and frequency differ.
| Side‑Effect | Ticlopidine | Clopidogrel |
|---|---|---|
| Neutropenia / Agranulocytosis | 3‑5 % (serious) | 0.1 % (rare) |
| Gastro‑intestinal bleeding | 1‑2 % | 1‑2 % |
| Rash / Pruritus | 5‑7 % | 2‑4 % |
| Thrombotic thrombocytopenic purpura (TTP) | Very rare | Very rare |
Neutropenia and agranulocytosis are the deal‑breakers for ticlopidine. Because the bone‑marrow toxicity can be life‑threatening, guidelines now recommend routine blood‑count monitoring for the first three months of therapy. Clopidogrel’s safety record is much cleaner, and routine labs are not required.
Drug Interactions and Metabolic Considerations
Since both drugs are processed by CYP2C19, any medication that inhibits this enzyme will blunt their antiplatelet effect. However, clopidogrel’s reliance on multiple CYP isoforms makes it more vulnerable. Strong inhibitors like fluoxetine, ketoconazole, or even certain proton‑pump inhibitors (e.g., omeprazole) can reduce clopidogrel’s active metabolite formation by up to 40 %.
Ticlopidine, on the other hand, is primarily a CYP2C19 substrate and is less affected by CYP3A4 inhibitors. Still, it induces CYP2C9 and CYP3A4, which can lower the concentrations of warfarin and certain statins, requiring dose adjustments.
Cost and Accessibility in the UK
As of October 2025, ticlopidine is marketed under the brand name Ticlid and is only available as a generic tablet. The NHS tariff lists it at £0.12 per 250 mg tablet. Clopidogrel, sold as Plavix and various generics, averages £0.15 per 75 mg tablet. While the price gap is small, the need for blood‑count monitoring with ticlopidine adds indirect costs-extra clinic visits, lab tests, and possible hospital admissions for severe neutropenia.
Guideline Recommendations
Current British Cardiovascular Society (BCS) guidelines (2024 edition) list clopidogrel as the preferred P2Y12 inhibitor for most patients after an acute coronary syndrome (ACS) or PCI, unless contraindicated. Ticlopidine is mentioned only as an alternative when clopidogrel is unavailable or when a patient has a documented CYP2C19 loss‑of‑function allele that reduces clopidogrel’s efficacy.
For patients with chronic kidney disease (CKD) stage 4‑5, ticlopidine may be considered because its active metabolite is less dependent on renal clearance, but the hematologic risks still dominate the decision.
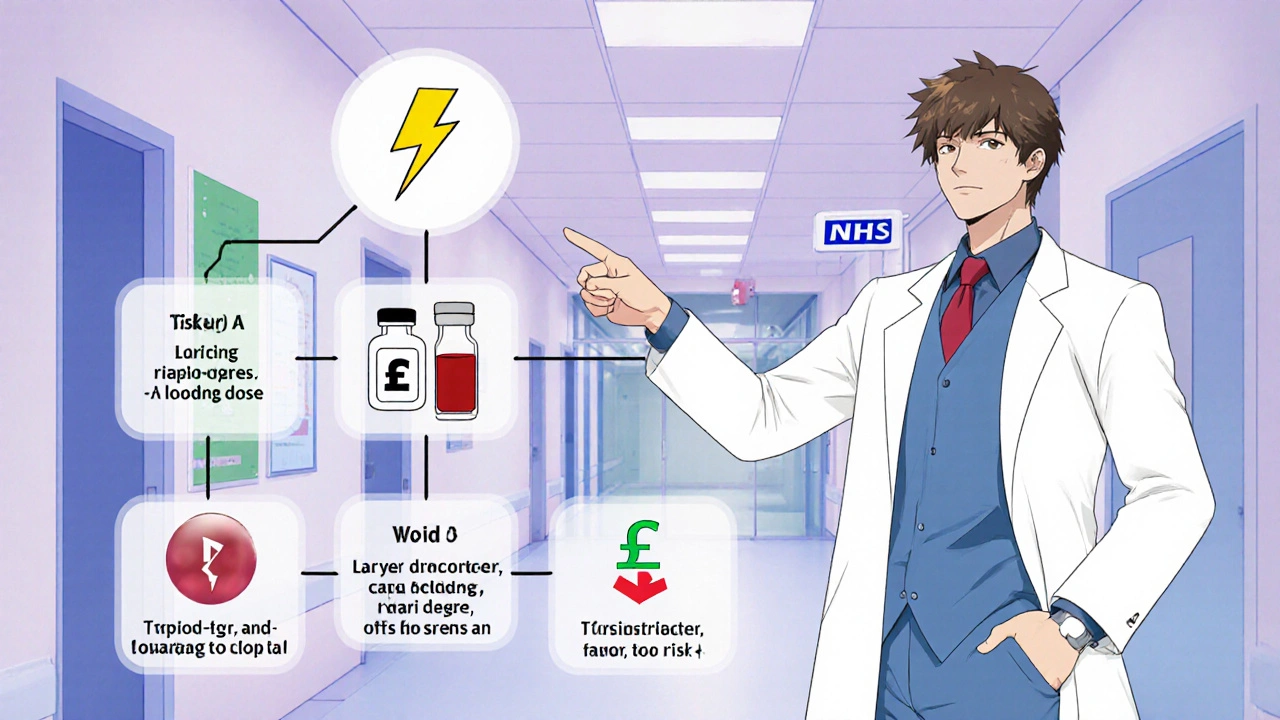
Choosing the Right Agent - A Practical Decision Tree
- Is rapid platelet inhibition required (e.g., after PCI)?
- Yes → Prefer clopidogrel with a loading dose.
- No → Continue to step 2.
- Does the patient have a history of neutropenia, agranulocytosis, or severe bone‑marrow disorders?
- Yes → Avoid ticlopidine.
- No → Continue to step 3.
- Is the patient taking strong CYP2C19 inhibitors?
- Yes → Ticlopidine may be less affected, but watch for drug‑induced liver enzyme changes.
- No → Clopidogrel remains the first‑line choice.
- Can the patient commit to regular blood‑count monitoring?
- Yes → Ticlopidine could be an option if cost is a major concern.
- No → Stick with clopidogrel.
This flowchart helps clinicians and patients weigh the trade‑offs without getting lost in jargon.
Real‑World Patient Stories
Sarah, a 68‑year‑old retired teacher from Bristol, was prescribed ticlopidine after a minor stroke in 2023 because her pharmacist ran out of clopidogrel. Within two weeks, she felt unusually fatigued, and a routine blood test revealed a white‑cell count of 2.1 × 10⁹/L. Her doctor switched her to clopidogrel, and her counts rebounded. Sarah’s experience illustrates why regular monitoring matters.
Conversely, Mark, a 55‑year‑old electrician with severe liver disease, could not tolerate clopidogrel due to elevated liver enzymes. His cardiologist opted for ticlopidine, coupled with weekly blood‑count checks. After three months, Mark remained clot‑free and had no hematologic issues, showing that ticlopidine can still be useful in niche scenarios.
Bottom Line - Which Drug Comes Out on Top?
If you boil everything down to efficacy, safety, convenience and cost, clopidogrel wins the majority vote. It offers faster onset, fewer severe blood‑disorders, and fits neatly into modern guidelines. Ticlopidine still has a place-especially where clopidogrel isn’t tolerated, where drug‑interaction profiles favor ticlopidine, or where cost constraints make the extra monitoring affordable.
In short, think of clopidogrel as the default antiplatelet for most patients. Keep ticlopidine in your back‑up toolbox for special cases, but always pair it with a strict blood‑count schedule.
Quick Reference Table
| Attribute | Ticlopidine | Clopidogrel |
|---|---|---|
| Year of FDA approval | 1991 | 1997 |
| Typical daily dose | 250 mg twice daily | 75 mg once daily (or 300 mg loading) |
| Onset of action | 3‑5 days | 4‑6 hrs after loading |
| Half‑life of active metabolite | 12‑14 hrs | 8 hrs |
| Primary metabolic pathway | CYP2C19 | CYP2C19, CYP3A4, CYP2B6 |
| Neutropenia / Agranulocytosis | 3‑5 % | ~0.1 % |
| GI bleeding risk | 1‑2 % | 1‑2 % |
| Drug‑interaction sensitivity | Moderate (CYP2C19 inhibitors) | High (CYP2C19 & CYP3A4 inhibitors) |
| Monitoring requirement | CBC every 2‑3 weeks for 3 months | None required |
| Average UK cost (per tablet) | £0.12 | £0.15 |
Frequently Asked Questions
Can I switch from ticlopidine to clopidogrel without a wash‑out period?
Yes. Because both drugs bind irreversibly to the same receptor, you can stop ticlopidine and start clopidogrel the next day. However, keep an eye on platelet function tests for the first week if you’re in a high‑risk setting.
Is genetic testing for CYP2C19 useful before choosing a drug?
For clopidogrel, a loss‑of‑function CYP2C19 allele can blunt its effect, so testing is recommended in patients with recurrent events despite therapy. Ticlopidine’s activation is less affected by these variants, making it an alternative if testing shows poor metabolism.
What should I do if I develop a rash while on either medication?
Stop the drug and contact your prescriber immediately. A rash could be an early sign of hypersensitivity, and both agents can cause severe skin reactions in rare cases.
Are there any dietary restrictions with ticlopidine or clopidogrel?
No specific foods need to be avoided, but limit grapefruit juice if you’re on clopidogrel because it can inhibit CYP3A4 and affect drug levels. Alcohol in excess can increase bleeding risk with both drugs.
Can I take aspirin together with either drug?
Yes, many cardiology protocols use low‑dose aspirin (75‑81 mg) plus a P2Y12 inhibitor. This dual antiplatelet therapy (DAPT) lowers clot risk after stent placement, but it also raises bleeding risk, so follow your doctor’s dosing schedule closely.
How often should I get blood work if I’m on ticlopidine?
Guidelines suggest a complete blood count (CBC) every 2‑3 weeks for the first three months, then monthly for another three months. After six months, if counts are stable, testing can be spaced out to every 6‑12 months.
Is clopidogrel safe during pregnancy?
Clopidogrel is classified as FDA pregnancy category B, meaning animal studies showed no risk but there are no well‑controlled human studies. It should only be used if the benefit outweighs potential risk, and under specialist guidance.
Peter Richmond
October 23, 2025 AT 12:53Clopidogrel’s faster onset and cleaner safety profile make it the pragmatic choice for most clinicians, especially when rapid platelet inhibition is needed after PCI.
Jinny Shin
October 24, 2025 AT 16:39One cannot help but note the subtle elegance of ticlopidine’s pharmacology, a relic of an earlier era that still whispers its relevance amidst the chorus of modern agents.
deepak tanwar
October 25, 2025 AT 20:26While cost differences appear negligible, the hidden expenses of routine CBC monitoring for ticlopidine often outweigh any modest savings, rendering the purported economic advantage illusory.
Vikas Kumar
October 26, 2025 AT 23:13India’s guidelines still list clopidogrel as first‑line, reflecting global consensus.
Celeste Flynn
October 28, 2025 AT 02:59For patients worried about drug interactions, remember that strong CYP2C19 inhibitors can blunt both drugs but the effect is more pronounced with clopidogrel so check meds before prescribing.
Shan Reddy
October 29, 2025 AT 06:46Just a heads‑up: ticlopidine needs blood‑count checks, clopidogrel doesn’t – that’s a big convenience factor.
Zachary Blackwell
October 30, 2025 AT 10:33Ever wonder why pharma pushes clopidogrel so hard? Some say it’s all about patent extensions and big‑pharma profit motives – keep an eye on the agenda.
prithi mallick
October 31, 2025 AT 14:19Its important to remember that whichever drug you pick, the ultimate goal is your health – stay positive and keep in touch with your doc.
Michaela Dixon
November 1, 2025 AT 18:06When you dive into the labyrinthine world of antiplatelet therapy, the first thing that strikes you is the sheer complexity of metabolic pathways, each twist and turn unveiling a fresh cascade of enzymatic interactions that can tip the balance between therapeutic success and adverse events; ticlopidine, for instance, dances primarily with CYP2C19, a partnership that, while elegant, can be disrupted by a host of other medications, whereas clopidogrel waltzes through a more intricate choreography involving CYP2C19, CYP3A4, and CYP2B6, making it a more finicky performer on the pharmacological stage; this very intricacy manifests clinically as a heightened sensitivity to drug‑drug interactions, especially with proton‑pump inhibitors like omeprazole, which can blunt clopidogrel’s antiplatelet punch by as much as forty percent, a fact that cannot be ignored when tailoring therapy for patients juggling multiple prescriptions; yet, the narrative does not end there, because the safety profile of these agents adds another layer to the decision‑making matrix, with ticlopidine bearing the notorious burden of neutropenia and agranulocytosis, complications that demand vigilant blood‑count monitoring and can occasionally culminate in life‑threatening scenarios, a stark contrast to clopidogrel’s comparatively benign haematologic footprint; nevertheless, cost considerations weave their own thread into this tapestry, where the marginal price difference between the generic forms becomes almost negligible when one factors in the ancillary expenses of laboratory testing and potential hospitalizations associated with ticlopidine’s hematologic toxicity; beyond the hard data, patient stories breathe life into these statistics, as exemplified by Sarah’s experience of fatigue and leukopenia that prompted a swift switch to clopidogrel, underscoring the real‑world impact of vigilant monitoring, while Mark’s tale highlights that in niche populations-such as those with severe liver disease-ticlopidine can still carve out a therapeutic niche when clopidogrel proves intolerable; guidelines, too, have spoken, with the British Cardiovascular Society favoring clopidogrel as the default P2Y12 inhibitor for acute coronary syndromes and post‑PCI scenarios, relegating ticlopidine to a backup role reserved for specific circumstances like CYP2C19 loss‑of‑function genotypes or cost‑driven constraints; nonetheless, the decision matrix remains fluid, and clinicians must weigh the urgency of platelet inhibition, the patient’s comorbid profile, potential drug interactions, and the feasibility of regular laboratory surveillance before arriving at the optimal choice; in the end, the art of medicine lies in harmonizing evidence‑based guidelines with individual patient nuances, ensuring that the selected antiplatelet agent not only mitigates thrombotic risk but also aligns with the patient’s lifestyle, preferences, and capacity for follow‑up care.
Dan Danuts
November 2, 2025 AT 21:53Great summary! If you’re on a tight budget, ticlopidine can be a cost‑effective alternative-just remember those blood‑work appointments.
Dante Russello
November 4, 2025 AT 01:39Indeed, the comprehensive overview you provided highlights the multifaceted considerations-efficacy, safety, pharmacogenomics, and health‑system logistics-all of which must be balanced; for clinicians mentoring trainees, emphasizing the importance of regular CBC monitoring with ticlopidine can reinforce good clinical habits, while also underscoring that, in many cases, clopidogrel’s ease of use and favorable safety profile may streamline patient management and improve adherence.