Lupus Therapy Suitability Checker
Find Your Best Complementary Therapy Matches
Answer a few questions about your lupus symptoms, medications, and lifestyle to identify therapies that may work well for you. Always discuss with your rheumatologist before starting new therapies.
Current Symptoms
Current Medications
Lifestyle Considerations
Recommended Complementary Therapies
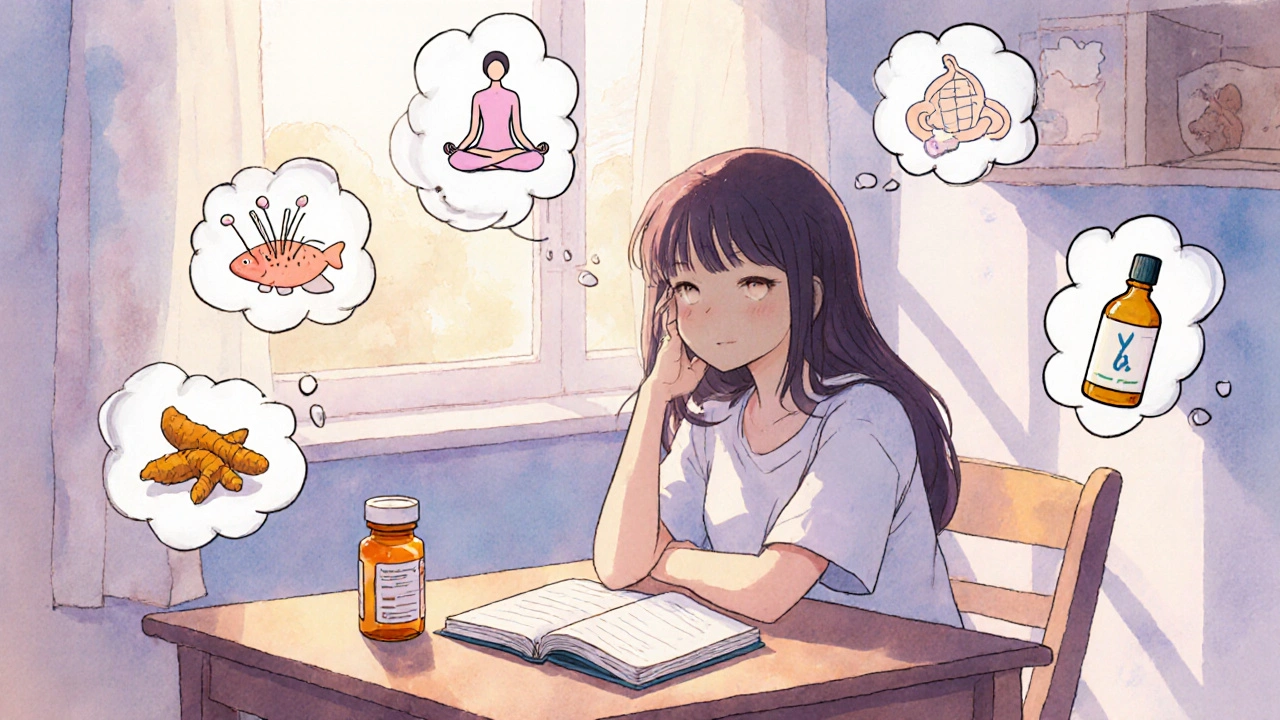
Living with Lupus is an autoimmune condition that can cause fatigue, joint pain, skin rashes, and organ inflammation often feels like a constant juggling act between medication, flare‑ups, and everyday life. While conventional drugs are essential for controlling disease activity, many patients ask: can I add anything else that won’t clash with my prescription and might ease symptoms?
That’s where alternative therapies for lupus come in. Below you’ll find a practical rundown of the most studied natural approaches, clear guidance on safety, and tips for weaving them into a balanced lupus‑care plan.
Understanding Lupus and Its Treatment Landscape
Before diving into herbs or mind‑body practices, it helps to recap what lupus does at the cellular level. The immune system mistakenly creates auto‑antibodies that attack healthy tissue, triggering inflammation. Standard treatments-corticosteroids, antimalarials, immunosuppressants-target this over‑active response. However, these drugs can bring side effects like weight gain, bone loss, or increased infection risk.
Because lupus is a systemic disease, a one‑size‑fits‑all plan rarely works. Many clinicians now endorse a “holistic” approach: combine evidence‑based medicine with lifestyle tweaks, nutrition, and safe complementary modalities.
Why Look Beyond Prescription Medicines?
- Symptom relief: Some natural therapies can reduce fatigue, improve sleep, or calm joint pain without adding another pill.
- Reduced drug burden: When safe, adjuncts may allow lower doses of steroids, limiting long‑term complications.
- Empowerment: Active self‑care fosters a sense of control, which can positively affect mood and disease perception.
That said, not every alternative option is suitable for every patient. The key is evaluating evidence, checking for interactions, and consulting your rheumatologist before starting anything new.
Top Natural Options Backed by Research
Below are the most commonly recommended therapies, each introduced with its own microdata tag for easy knowledge‑graph extraction.
Acupuncture
Acupuncture involves inserting thin needles at specific points to modulate nerve signals and promote endorphin release. Small pilot studies in lupus patients report modest reductions in pain scores and improved fatigue after 6‑8 weekly sessions.
Yoga
Yoga blends gentle stretches, breathing, and meditation. A 2021 randomized trial showed that a 12‑week yoga program lowered disease activity indices (SLEDAI) and improved sleep quality compared with a control group.
Omega‑3 Fatty Acids
Found in fish oil, EPA and DHA have anti‑inflammatory properties. Meta‑analyses reveal that regular omega‑3 supplementation can modestly reduce joint swelling and corticosteroid requirements in lupus.
Turmeric (Curcumin)
Curcumin, the active compound in turmeric, inhibits NF‑κB pathways that drive inflammation. Small human studies suggest it can lower C‑reactive protein levels and improve skin rash severity when taken as a 500 mg capsule twice daily.
Vitamin D
Vitamin D deficiency is common in lupus due to photosensitivity and steroid use. Adequate levels (≥30 ng/mL) are linked to fewer flares and better bone health. Supplementation of 1,000-2,000 IU per day is generally safe, but blood monitoring is advised.
Probiotics
Gut dysbiosis may aggravate autoimmune activity. Certain probiotic strains (Lactobacillus rhamnosus, Bifidobacterium longum) have shown promise in reducing systemic inflammation markers in small lupus cohorts.
Mind‑Body Practices (Meditation)
Mindfulness meditation, guided imagery, and progressive muscle relaxation can lower perceived stress-a known trigger for lupus flares. A 2022 systematic review found meditation reduced fatigue scores by an average of 12 %.
Cat’s Claw (Uncaria tomentosa)
Cat’s claw is a South‑American vine reputed for immunomodulatory effects. Preliminary in‑vitro work suggests it may down‑regulate cytokine production, but human data remain limited, so caution is advised.

Evidence & Safety - How to Choose the Right Fit
When evaluating any alternative therapy, ask three simple questions:
- What’s the quality of evidence? Look for randomized controlled trials (RCTs) or systematic reviews rather than anecdotal claims.
- Are there known interactions? For instance, high doses of fish oil may increase bleeding risk when combined with anticoagulants.
- Is the intervention realistic for my lifestyle? A therapy that requires daily 1‑hour sessions may be unsustainable for a working parent.
Always discuss these points with your rheumatologist. They can help monitor lab values, adjust medication dosages, and flag any red flags.
Quick Comparison of Popular Options
| Therapy | Evidence Level | Typical Benefits | Potential Risks / Interactions | Ease of Use |
|---|---|---|---|---|
| Acupuncture | Low‑to‑moderate (small RCTs) | Pain relief, reduced fatigue | Minor bruising; avoid if on blood thinners | Clinic visits, 30‑min weekly |
| Yoga | Moderate (single RCT) | Improved flexibility, mood, sleep | Joint strain if poses are aggressive | Home practice possible, 20‑30 min/day |
| Omega‑3 Fatty Acids | Moderate (meta‑analysis) | Lower inflammation, joint swelling | Bleeding risk at high doses | Daily supplement, easy |
| Turmeric (Curcumin) | Low (small trials) | Skin rash improvement, pain | GI upset; may affect blood thinners | Capsule or spice, twice daily |
| Vitamin D | High (observational + supplementation studies) | Fewer flares, bone health | Hypercalcemia if overdosed | Daily pill, blood test monitoring |
| Probiotics | Low (pilot studies) | Gut health, reduced systemic markers | Rare GI upset | Daily capsule, easy |
| Meditation | Moderate (systematic review) | Stress reduction, fatigue | None | 5‑10 min/day, apps feasible |
| Cat’s Claw | Very low (in‑vitro, limited human data) | Potential immune modulation | Possible liver enzyme elevation | Herbal supplement, caution advised |

Practical Tips for Integrating Therapies Safely
- Start slow: Introduce one new modality at a time. Give your body 4‑6 weeks to adjust before adding another.
- Document changes: Keep a symptom diary noting pain levels, fatigue, and any side effects. This helps you and your doctor see what works.
- Check supplement purity: Choose products with third‑party testing (USP, NSF) to avoid contaminants.
- Timing matters: Take omega‑3s with meals to improve absorption; space vitamin D from high‑calcium foods if you have kidney concerns.
- Schedule regular labs: Monitor CBC, liver enzymes, and vitamin D levels every 3-6 months when you add new supplements.
Common Pitfalls & Red Flags
Even well‑meaning natural approaches can backfire if misused. Watch out for these warning signs:
- Sudden increase in joint pain or new rashes after starting a supplement - stop and consult your doctor.
- Feeling overly drowsy from high‑dose fish oil - adjust dosage.
- Unusual bruising or bleeding - could be a sign of interaction with anticoagulants.
- Reliance on “cure‑all” herbs without medical supervision - lupus has no known cure, only management.
When in doubt, pause the therapy and seek professional advice. The goal is to complement, not replace, proven medications.
Frequently Asked Questions
Can I use acupuncture while on immunosuppressants?
Yes, acupuncture is generally safe with immunosuppressants, but avoid needling over active skin lesions and tell your practitioner about any bleeding disorders.
How much fish oil is enough for lupus?
Research typically uses 2-3 grams of combined EPA/DHA per day. Start with 1 gram and increase gradually, checking with your doctor for any blood‑thinning concerns.
Is yoga safe during a flare?
Gentle, low‑impact yoga can help maintain mobility, but avoid deep twists or inversions that stress inflamed joints. Listen to your body and modify poses as needed.
Do probiotics actually affect lupus activity?
Current evidence is preliminary, but certain strains appear to lower inflammatory markers. They’re low‑risk, so many clinicians consider them a reasonable adjunct, especially if you have GI symptoms.
Should I stop vitamin D supplements if my level is high?
If blood tests show >60 ng/mL, reduce the dose or pause supplementation. Excess vitamin D can lead to hypercalcemia, which may worsen kidney involvement.
Exploring alternative and complementary therapies can give you extra tools to manage lupus, but the foundation remains your prescribed medication and regular doctor visits. Use the information above to have an informed conversation with your healthcare team and build a personalized, safe plan.
Ralph Barcelos de Azevedo
October 21, 2025 AT 21:04While it’s tempting to chase every shiny supplement, the first duty we owe ourselves is to ensure nothing jeopardises the hard‑won stability of our lupus regimen. Evidence‑based therapies should remain the backbone, and any add‑on must be vetted for drug interactions. For instance, high‑dose fish oil can thin the blood, which is a red flag for patients on anticoagulants. Keep a meticulous log of what you take, and bring it to every rheumatology visit. Safety first, curiosity second.
Peter Rupar
October 24, 2025 AT 09:04Yo, stop acting like every herbal tea is a miracle cure – you’ll end up with a busted immune system and a wallet full of junk. People throw around “natural” like it’s a free pass, but most of that stuff is untested garbage. If you’re not willing to read the fine print, just stick to your meds and quit the fairy‑tale hype. No one needs another anecdote‑driven disaster story on this thread.
Raja M
October 26, 2025 AT 20:04Living with lupus is like navigating a stormy sea while trying to read a map that keeps changing its ink. Every flare reminds us that the body is not just a machine but a conversation between cells, hormones, and our environment. When we open ourselves to complementary practices, we are essentially adding new words to that dialogue, hoping they translate into calmer waters. Acupuncture, for example, can be viewed as a subtle re‑wiring of neural pathways, sending signals that temper pain without flooding the system with chemicals. Yoga offers more than flexibility; it cultivates breath awareness that can dampen the stress‑induced spikes that often precede flares. Omega‑3 fatty acids act as gentle diplomats, coaxing inflammatory messengers to step back and let healing take the stage. Curcumin, the golden pigment of turmeric, has been shown to mute the NF‑κB orchestra that drives much of the autoimmune cacophony. Vitamin D, though simple, plays a starring role in regulating immune tolerance, and a deficiency is like removing the conductor from an already chaotic symphony. Probiotics whisper to our gut, reminding it that balance is possible even when the rest of the body feels out of sync. Mindfulness meditation, with its quiet focus, can lower the cortisol tide that fuels flare‑ups, acting as a mental ballast. Even the more obscure cat’s claw, when used cautiously, offers a glimpse into how ancient botanicals might modulate immune signaling. The common thread among these therapies is intention: we are not trying to replace prescription drugs, but to create a supportive ecosystem around them. That ecosystem thrives on evidence, communication with healthcare providers, and a realistic assessment of what fits into one’s daily life. Patience and consistent monitoring are the compass that will guide us through this integrated approach.
Rob Flores
October 29, 2025 AT 08:04Ah, the ever‑expanding list of “natural miracles” – because why settle for evidence when you can parade a bottle of turmeric like it’s a Nobel prize? If you enjoy sprinkling jargon over a salad while ignoring the pharmacokinetics, go ahead, but don’t expect the scientific community to applaud your culinary experiments.
Shiv Kumar
October 31, 2025 AT 20:04One must acknowledge that the appeal of alternative modalities often stems from a desire for agency, yet the literature still favors rigor over anecdote. Selecting supplements that are third‑party verified can mitigate the risk of contamination, a point worth noting for the discerning reader.
Ryan Spanier
November 3, 2025 AT 08:04It’s encouraging to see the community emphasize documentation; keeping a symptom diary can truly illuminate which adjuncts prove beneficial. I recommend recording pain scores, fatigue levels, and sleep quality alongside any new supplement, then reviewing the trends with your rheumatologist every few months. This systematic approach not only fosters collaboration with your care team but also empowers you with concrete data to make informed decisions.
Abhinav Moudgil
November 5, 2025 AT 20:04Think of your wellness plan as a vibrant palette – a dash of omega‑3 here, a swirl of yoga there, and a bright splash of vitamin D to brighten the whole picture. By layering these evidence‑backed strokes, you create a masterpiece that supports your body without painting over the essential prescription base.
Miah O'Malley
November 8, 2025 AT 08:04In the grand tapestry of health, each thread – whether pharmaceutical or herbal – contributes to the overall design. Recognizing the interdependence of mind, gut, and immune system invites us to weave a more resilient fabric, one that can better withstand the inevitable wear of disease.
Bradley Allan
November 10, 2025 AT 20:04Wow!!! This guide just blew my mind!!!
Kyle Garrity
November 13, 2025 AT 08:04I hear you, the sheer volume of options can feel overwhelming, especially when every new study promises a miracle. Remember that personal experience matters, so give yourself permission to trial one approach at a time and observe how you feel. Consistency, not complexity, often yields the most sustainable results.
brandon lee
November 15, 2025 AT 20:04yeah just pick something lowkey like a short daily meditation and see if it helps your stress levels it’s a simple start that doesn’t cost much
Joshua Pisueña
November 18, 2025 AT 08:04Start with a quality fish oil capsule take it with breakfast and track any changes you notice it’s a small step that can add up
Nikita Shue
November 20, 2025 AT 20:04Make sure the dosage isn’t too high if you’re on blood thinners – a quick check with your doctor will keep you from accidental bleeding and keep the benefits rolling.