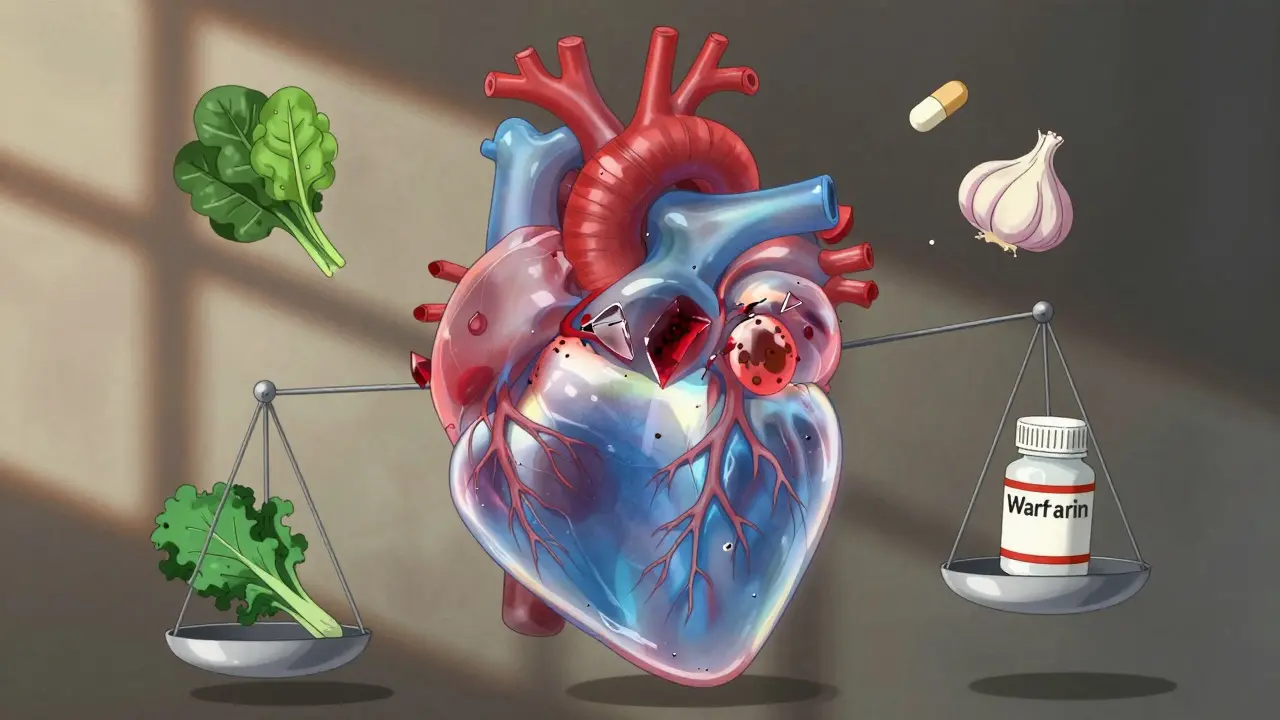
Warfarin is one of the oldest and most widely used blood thinners in the world. It’s cheap, effective, and has saved millions of lives since the 1950s. But here’s the catch: warfarin doesn’t play well with much of anything else. A single change in your diet, a new supplement, or even a common antibiotic can send your INR levels skyrocketing-or crashing. And when that happens, the risks aren’t theoretical. You could bleed internally, have a stroke, or end up in the ER. This isn’t scare tactics. It’s fact. If you’re on warfarin, you need to know exactly what to avoid-and what to keep consistent.
How Warfarin Actually Works
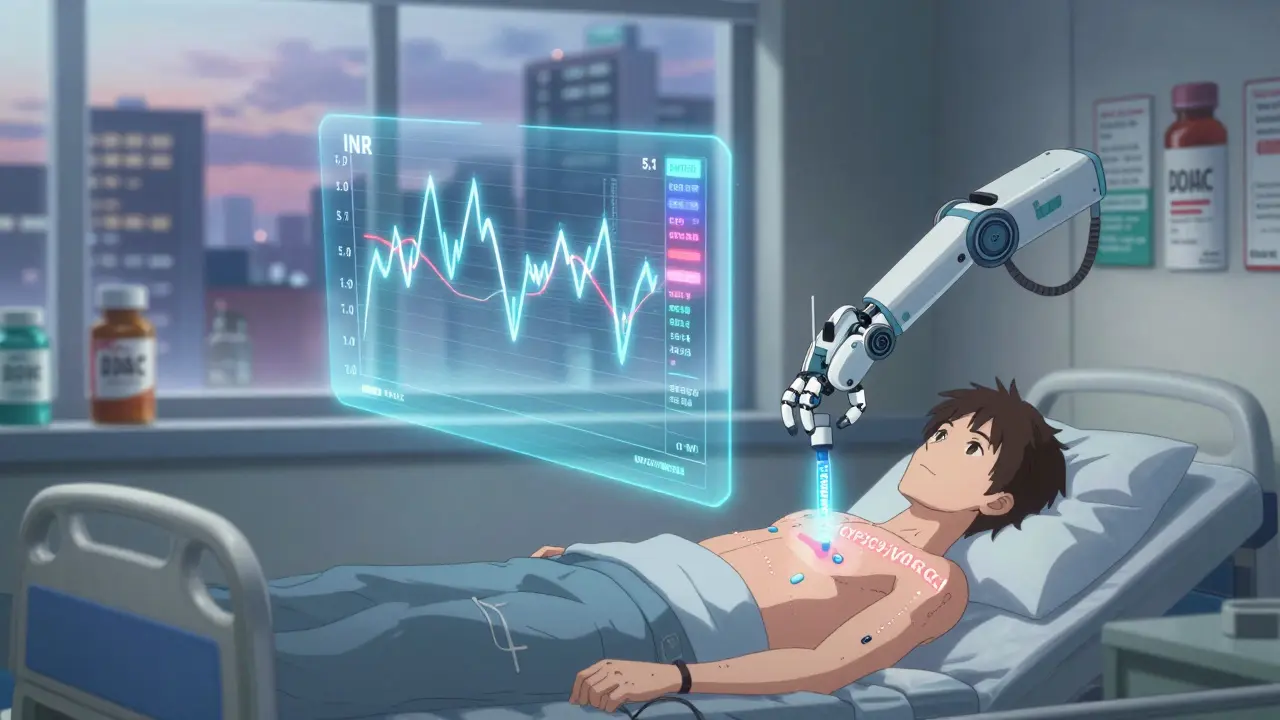
Warfarin doesn’t thin your blood like water. Instead, it blocks vitamin K from doing its job. Vitamin K is essential for making proteins that help your blood clot. Without enough active vitamin K, your blood takes longer to clot. That’s the goal. But it’s a tightrope walk. Too little clotting, and you risk dangerous bleeding. Too much, and you risk clots forming in your heart, lungs, or brain. Your doctor keeps your INR (International Normalized Ratio) between 2.0 and 3.0. If you’re on a mechanical heart valve, they might aim higher-2.5 to 3.5. But that number changes fast. One week you’re stable. The next, your INR jumps from 2.3 to 5.1 because you ate a big salad or took a new painkiller.
Foods That Mess With Warfarin: It’s All About Vitamin K
You don’t have to give up greens. But you must keep them consistent. The biggest mistake people make? Eating a ton of spinach on Monday, then skipping it for a week. That’s a recipe for unstable INR.
Vitamin K is found mostly in leafy greens, but also in broccoli, Brussels sprouts, cabbage, and kale. Here’s what you’re really dealing with:
- 1 cup cooked spinach = 1,062 mcg vitamin K
- 1 cup cooked kale = 1,062 mcg
- 1 cup cooked broccoli = 220 mcg
- 1 cup raw lettuce = 30 mcg
- 1 egg = 0.3 mcg
That’s a 3,500% difference between spinach and lettuce. If you suddenly start eating two cups of spinach daily, your INR can drop by 0.5 to 1.5 within just 3 to 5 days. That means your blood clots faster. Your doctor might increase your warfarin dose, only for you to swing back the other way when you eat less.
Experts recommend keeping your daily vitamin K intake steady-between 60 and 80 mcg per day. That’s roughly one serving of greens. Don’t go crazy. Don’t go cold turkey. Just keep it the same. One patient on Reddit said they eat exactly one cup of cooked spinach at 6 p.m. every day. That’s not an accident. That’s strategy.
Supplements That Can Be Dangerous
Just because it’s sold as a “natural supplement” doesn’t mean it’s safe with warfarin. In fact, many are far more dangerous than prescription drugs.
- St. John’s Wort: This herb for depression can cut warfarin’s effectiveness by up to 60%. One study showed INR dropping from 2.8 to 1.4 within a week-putting the patient at immediate risk of clotting.
- Ginkgo biloba: Known to improve memory, but it also inhibits platelet function. Combined with warfarin, bleeding risk jumps 3.4 times. ER visits from this combo are not rare.
- Ginseng: Can either increase or decrease warfarin’s effect. No one can predict which. The safest answer? Avoid it.
- Garlic supplements: While eating garlic in food is fine, concentrated pills can increase bleeding risk. One 2021 study found 28% of patients on garlic supplements had INR levels above 4.0.
- Vitamin E: High doses (over 400 IU/day) interfere with clotting. A single 1,000 IU capsule can push your INR into dangerous territory.
- Coenzyme Q10: Some reports suggest it may reduce warfarin’s effect. Not well studied, but enough cases exist to warrant caution.
The National Blood Clot Alliance found that 24% of warfarin users had a major interaction from supplements. Most didn’t even tell their doctor they were taking them. Don’t be one of them.

Prescription Drugs That Interact-And How Bad It Gets
Warfarin has over 300 known drug interactions. That’s 10 times more than newer blood thinners like Eliquis or Xarelto. Here are the big ones you absolutely need to watch for:
- Antibiotics: Especially trimethoprim-sulfamethoxazole (Bactrim) and ciprofloxacin (Cipro). These can increase warfarin levels by 50-100%. One patient reported their INR jumped from 2.4 to 5.1 after a single course of Bactrim. That’s a 112% increase in bleeding risk. Always tell your pharmacist you’re on warfarin before taking any antibiotic.
- Fluconazole (Diflucan): An antifungal used for yeast infections. It blocks the liver enzyme that breaks down warfarin. INR can spike within 48 hours. Doctors often reduce warfarin dose by 25-50% when prescribing this.
- Amiodarone: Used for heart rhythm problems. It’s one of the most dangerous combinations. It can double warfarin’s effect. Patients on this combo often need weekly INR checks.
- NSAIDs: Ibuprofen, naproxen, celecoxib. These don’t change warfarin levels, but they irritate the stomach lining. Add that to warfarin’s thinning effect, and you’ve got a recipe for internal bleeding. Acetaminophen (Tylenol) is safer for pain.
- SSRIs: Antidepressants like fluoxetine (Prozac) and sertraline (Zoloft) can increase bleeding risk by 30-40%. If you’re on one, your doctor should monitor your INR more closely.
- Aspirin: Even low-dose aspirin (81 mg) increases bleeding risk. It’s not always avoided, but only if the benefit clearly outweighs the risk-like after a heart attack. Never start aspirin on your own.
Here’s the hard truth: 84% of reported warfarin interactions come from case studies with small numbers. But some interactions? They’re rock solid. Fluconazole. Bactrim. Amiodarone. These aren’t myths. They’re clinical realities.
Alcohol, Smoking, and Other Lifestyle Factors
Alcohol is tricky. One or two drinks a night? Probably fine. Three or more? That triples your bleeding risk. Chronic heavy drinking can also damage your liver, which is where warfarin is processed. That means your body can’t clear it properly-leading to dangerous buildup.
Smoking? It speeds up how fast your liver breaks down warfarin. If you quit smoking, your INR can rise without any change in dose. One study found INR increased by 0.8 within two weeks after quitting. That’s enough to cause bleeding. Tell your doctor if you’re quitting smoking.
And don’t forget about herbal teas. Green tea, in particular, has been linked to lower INR. One patient on a patient forum said their INR dropped from 2.8 to 1.9 after drinking 3 cups a day. Their doctor had to increase their warfarin dose by 20%.
What You Can Do: A Practical Game Plan
Managing warfarin isn’t about fear. It’s about consistency. Here’s what works:
- Keep your vitamin K intake steady. Eat the same amount of greens every day. Don’t go on a kale kick. Don’t skip them for a week. One serving, daily.
- Never start a new supplement without asking your doctor. Even “harmless” ones like fish oil or multivitamins. Some have hidden vitamin K or antiplatelet effects.
- Always tell every doctor, dentist, and pharmacist you’re on warfarin. Even for a simple UTI. A single antibiotic can change everything.
- Use a blood thinner tracker. Write down what you eat, what meds you take, and your INR number. Patterns show up fast. One patient noticed their INR dropped every time they had Chinese food-turns out, the stir-fry had a ton of leafy greens.
- Know the signs of bleeding. Unexplained bruising, nosebleeds that won’t stop, blood in urine or stool, severe headaches, or dizziness. Call your doctor immediately.
- Get your INR checked regularly. Even if you feel fine. Stable doesn’t mean safe. It means you haven’t changed anything yet.
Warfarin vs. Newer Blood Thinners: Is It Time to Switch?
DOACs like apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) don’t need diet changes, don’t need regular blood tests, and have fewer interactions. So why do so many people still take warfarin?
Three reasons:
- Cost. Warfarin costs $4-$10 a month. Eliquis costs $6,500 a year. For Medicare patients, 40% pay $0 for warfarin. Only 20% pay $0 for DOACs.
- Reversibility. If you bleed, vitamin K or a blood product can reverse warfarin in hours. DOACs have reversal agents too, but they’re expensive and not always available.
- Specific conditions. If you have a mechanical heart valve, antiphospholipid syndrome, or severe kidney failure, DOACs aren’t approved. Warfarin is your only option.
For most people without these conditions, DOACs are safer and easier. But if cost, access, or your specific health issue keeps you on warfarin, you can still manage it safely. Just don’t ignore the rules.
What’s Next? Genetic Testing and AI
In 2023, the FDA approved a new test called Warfarin GenAssist. It checks your genes-CYP2C9 and VKORC1-to predict how you’ll respond to warfarin. This can reduce the time to reach stable INR by over two weeks. It’s not perfect, but it helps. In trials, patients using this test needed fewer dose changes and fewer ER visits.
And AI is coming. A 2023 study showed machine learning models could predict warfarin dose changes with 82% accuracy-far better than doctors using standard charts. These tools won’t replace your doctor, but they’ll help them make smarter decisions faster.
Warfarin isn’t going away. Not yet. But your job is simple: stay consistent, stay informed, and never assume something is harmless. Your life depends on it.
Can I eat leafy greens while on warfarin?
Yes-but only if you eat the same amount every day. Sudden changes in vitamin K intake cause INR swings. Stick to one serving (like one cup of cooked spinach or kale) daily. Don’t skip it, don’t double it. Consistency is more important than avoiding greens entirely.
Is it safe to take ibuprofen with warfarin?
No. Ibuprofen and other NSAIDs increase the risk of stomach bleeding when combined with warfarin. Even occasional use can be dangerous. Use acetaminophen (Tylenol) instead for pain or fever. Always check with your doctor before taking any painkiller.
Why do I need to get my INR checked so often?
Warfarin’s effect changes with diet, medications, illness, and even weather. Your INR can swing in days. Regular checks (every 4 weeks when stable) catch these changes before they cause bleeding or clots. Skipping tests is risky-even if you feel fine.
Can I drink alcohol while on warfarin?
One or two drinks occasionally is usually fine. But three or more per day triples your bleeding risk. Heavy drinking also damages your liver, which affects how your body processes warfarin. If you drink regularly, tell your doctor. They may need to check your INR more often.
Do all supplements interact with warfarin?
No-but many do. St. John’s Wort, ginkgo, garlic supplements, high-dose vitamin E, and ginseng are known to interfere. Even multivitamins can contain vitamin K. Always list every supplement you take to your doctor. Don’t assume it’s safe just because it’s natural.
Is warfarin being replaced by newer drugs?
Yes-for many people. DOACs like Eliquis and Xarelto don’t need diet changes or regular blood tests. But warfarin is still essential for those with mechanical heart valves, severe kidney disease, or antiphospholipid syndrome. Cost also plays a big role. For many, warfarin remains the only affordable option.
Annie Joyce
February 11, 2026 AT 20:40Yo, I’ve been on warfarin for 8 years and honestly? The biggest game-changer was just eating the same damn spinach salad every night at 6 p.m. No more ‘I’ll have kale today’ then ‘nah, I’m tired’ tomorrow. Consistency is king. My INR went from rollercoaster to stable as a rock. Also, I started using a little food tracker app - it’s dumb, but it works. You don’t need to be a scientist, just a slightly obsessive person who likes routine. 😎